More than scales: the impact of obesity report
Written by:
-2.png&w=3840&q=75)
07 Jan 2026 • 67 min read
Reviewed and fact-checked:
.png&w=3840&q=75)
The challenges of obesity in the UK
Obesity costs the NHS billions each year and continues to shape long-term health outcomes nationwide. Yet despite its scale, the national conversation often fails to reflect lived reality.
- More than 55% of people in the UK believe the way weight is discussed has become increasingly harmful in their lifetime.
Weight is not just about personal effort
It’s shaped by the environments people live in, the work they do, the food they can afford, the time they have, their mental health, and whether support feels accessible and judgment-free. When these factors are ignored, responsibility is misplaced and progress stalls.
To uncover what obesity really looks like today, the clinical team at myBMI surveyed 5,000 adults across the UK.
The findings reveal a complex and uneven picture:
- Weight gain is rising fastest among younger adults
- Financial pressure and declining mental health are closely linked to changes on the scales
- Experiences of obesity vary sharply by region and gender
- Responses to obesity are changing, of the 5000 we surveyed, 1,000 are currently using, having used, or considering prescribed medication as part of a medically supported approach to weight management.
Together, these insights form the foundation of this report.
They show why obesity cannot be understood through numbers alone, and why meaningful progress depends on addressing the realities shaping people’s everyday lives.
In this report:
- Why obesity matters beyond the scales
- The state of weight in the UK
- The impact of weight on mental wellbeing
- The heavy pressures of everyday life
- The barriers to healthy lifestyle choices
- Our impact on the next generation
- Understanding weight behaviours
- Weight loss motivations
- Changing attitudes to weight loss medication
- Education is key to unlocking more choice
- Celebrating the positive impact of weight loss on our health
- 2026: the year our relationship with weight changes
Part 1: Why obesity matters beyond the scales
“This report looks beyond outcomes to understand what sits underneath; the pressures, constraints, and realities shaping weight and health across the UK”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
At myBMI, we do not see obesity as a single outcome or a matter of personal choice. We see it as the result of many factors that affect how people live, feel, and make decisions about their weight. That is why this report is structured around the four pillars of weight loss that guide how we support our patients to make lasting change.
- Education: how informed people feel about weight loss, what they track, and where gaps in understanding hold them back.
- Nutrition: the role of cost, access, convenience, and beliefs about healthy eating.
- Movement: activity levels, confidence, and the real-world barriers that stop people from being more active.
- Medication: awareness, attitudes, access, and the lived impact of weight loss treatments.
Together, these pillars reflect how weight management actually works in real life, not in theory. This report brings those insights together to highlight where people are struggling, where support is falling short, and where change is possible.
It is not just a snapshot of the current landscape, but a catalyst for more informed, compassionate, and effective approaches to weight loss, rooted in how people really live.
What this looks like:
Throughout the report, results are broken down by key demographics, including age, gender, income, region, and relationship status. This makes it clearer to see how experiences and attitudes towards weight differ across the UK.
The aim is not to place blame or judge behaviour. Instead, our More Than the Scales report highlights where pressures exist, who feels them most, and how those pressures change depending on people’s circumstances. Presenting the data side by side supports more open and informed conversations about obesity, moving beyond the idea that weight is solely about willpower.
Because obesity is more than just a number on the scales. It is something shaped by environment, access to support, and our everyday realities.
Part 2: The state of weight in the UK
The impact of obesity cannot be understood through statistics alone. It starts with understanding people’s circumstances, where they are in life, the pressures they face, and how these shape their weight day to day.
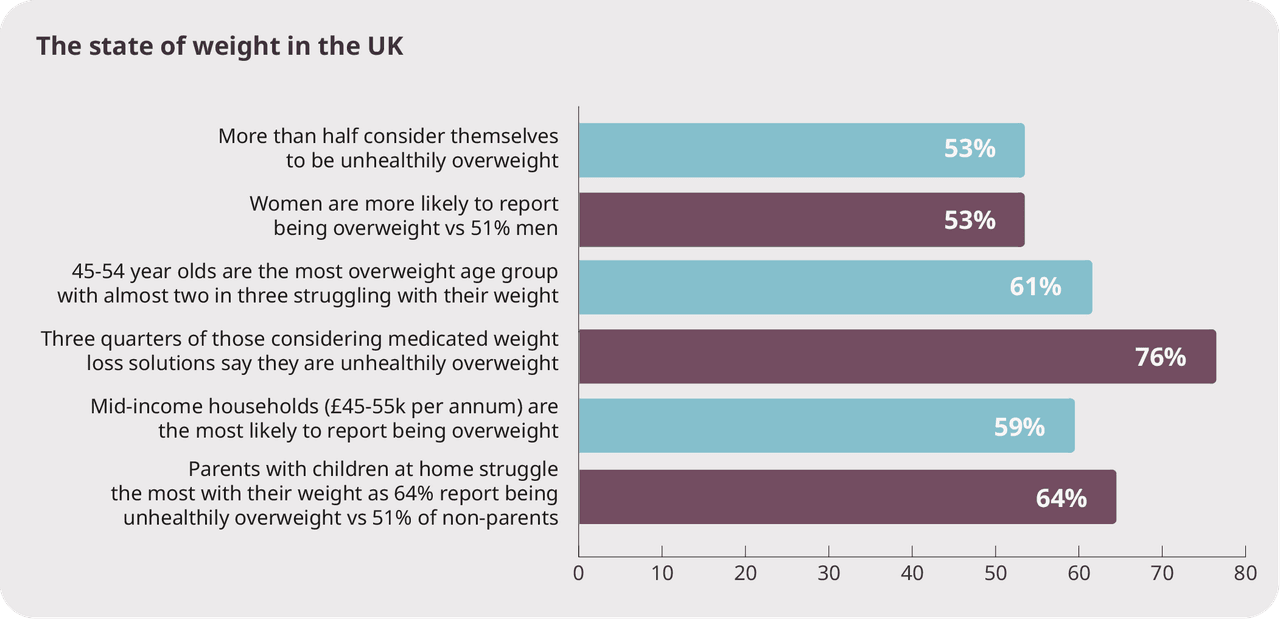
Right now, more than 53% of adults say they are unhealthily overweight. For many, this is not a passing concern, but an ongoing struggle shaped by daily pressures.
Weight challenges are most pronounced among:
- Women, who are slightly more likely than men to describe themselves as unhealthily overweight (53% vs 51%).
- Midlife adults, where almost two in three people aged 45–54 (61%) say they are struggling with their weight, often alongside work, family, and financial responsibilities.
Family and income pressures:
- Nearly two in three parents with children at home (64%) report being unhealthily overweight, compared with just over one in two (51%) people without children.
- Weight concerns cut across income levels, with those in mid-income households (£45–55k) the most likely to report being overweight (59%), challenging the idea that obesity affects only the lowest earners.
Growing need for medical support:
- Among people considering medicated weight loss, the need is clearest, with more than three quarters (76%) saying they are unhealthily overweight.
These figures show a country where weight struggles are common, uneven, and deeply tied to life stage, responsibility, and everyday pressure.
“What this data makes clear is that obesity doesn’t sit in isolation from the rest of someone’s life. Weight is shaped by work, family responsibilities, financial pressure, and where someone is in their personal journey. That’s why focusing on just one element rarely works. At myBMI, we see the best outcomes when people are supported across nutrition, movement, education, and, where appropriate, medication. It’s about meeting people where they are and giving them the tools that fit their reality, not asking them to work against it.”
Niya Mansuri, myBMI weight management and obesity expert
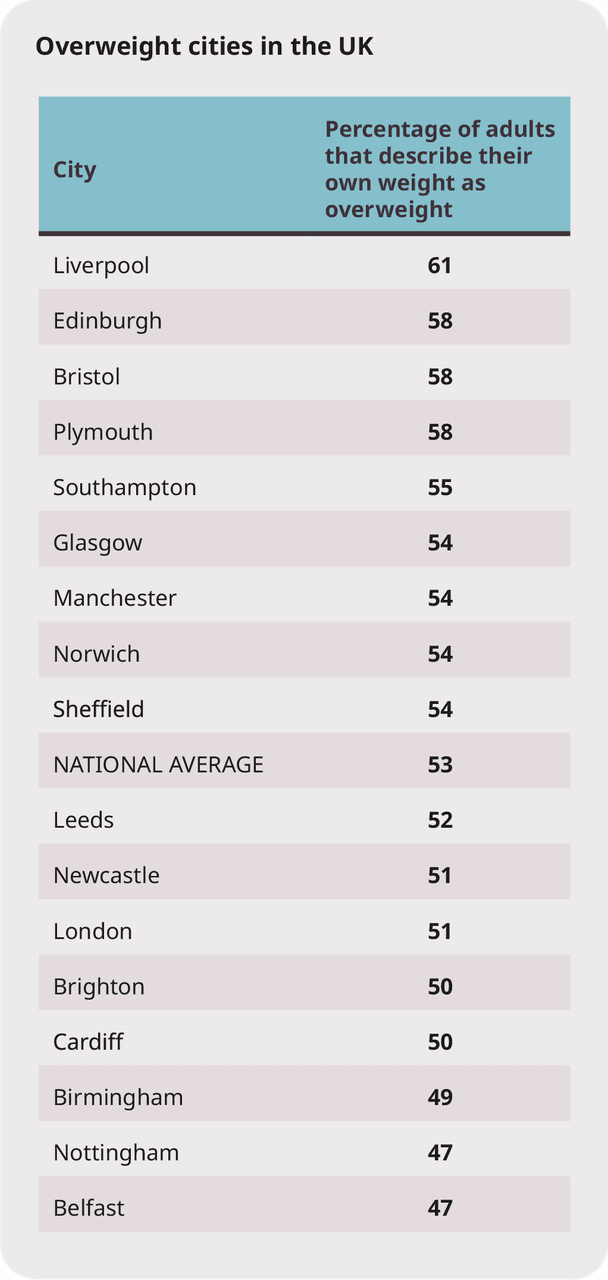
Across the UK, experiences of weight vary sharply by city. In Liverpool, more than three in five adults (61%) describe themselves as overweight, the highest of any city surveyed. Levels are also high in Edinburgh, Bristol, and Plymouth (58%), and remain above half in cities including Southampton, Glasgow, Manchester, Norwich, and Sheffield.
Elsewhere, rates sit closer to the midpoint. Around half of adults in Leeds, Newcastle, London, Brighton, and Cardiff describe themselves as overweight, while fewer than one in two do so in Birmingham, Nottingham, and Belfast.
Understanding where people live, and the pressures that come with it, is essential to understanding why obesity looks so different across the UK.
The UK is unhappy with its weight
Weight is not only a health issue, but an emotional one, shaped by pressure, comparison, and lived experience. Our data shows that for many people in the UK, that relationship is a difficult one.
.jpg&w=3840&q=75)
Less than 43% of adults say they are happy with their current weight, while almost one in three (28%) report feeling unhappy.
Happiness with weight varies sharply by group:
- Women are significantly less likely to feel positive about their weight, with just 38% reporting happiness compared with 49% of men.
Dissatisfaction peaks in midlife and family life:
- Only 27% of people aged 45–54 say they are happy with their weight, making this the least satisfied age group.
- Parents with children aged over 18 still at home report the lowest levels of happiness overall, with just 25% saying they are happy with their weight, compared with 29% of non-parents.
Weight dissatisfaction in the UK is widespread and closely linked to life stage, responsibility, and everyday pressure, not just health alone.
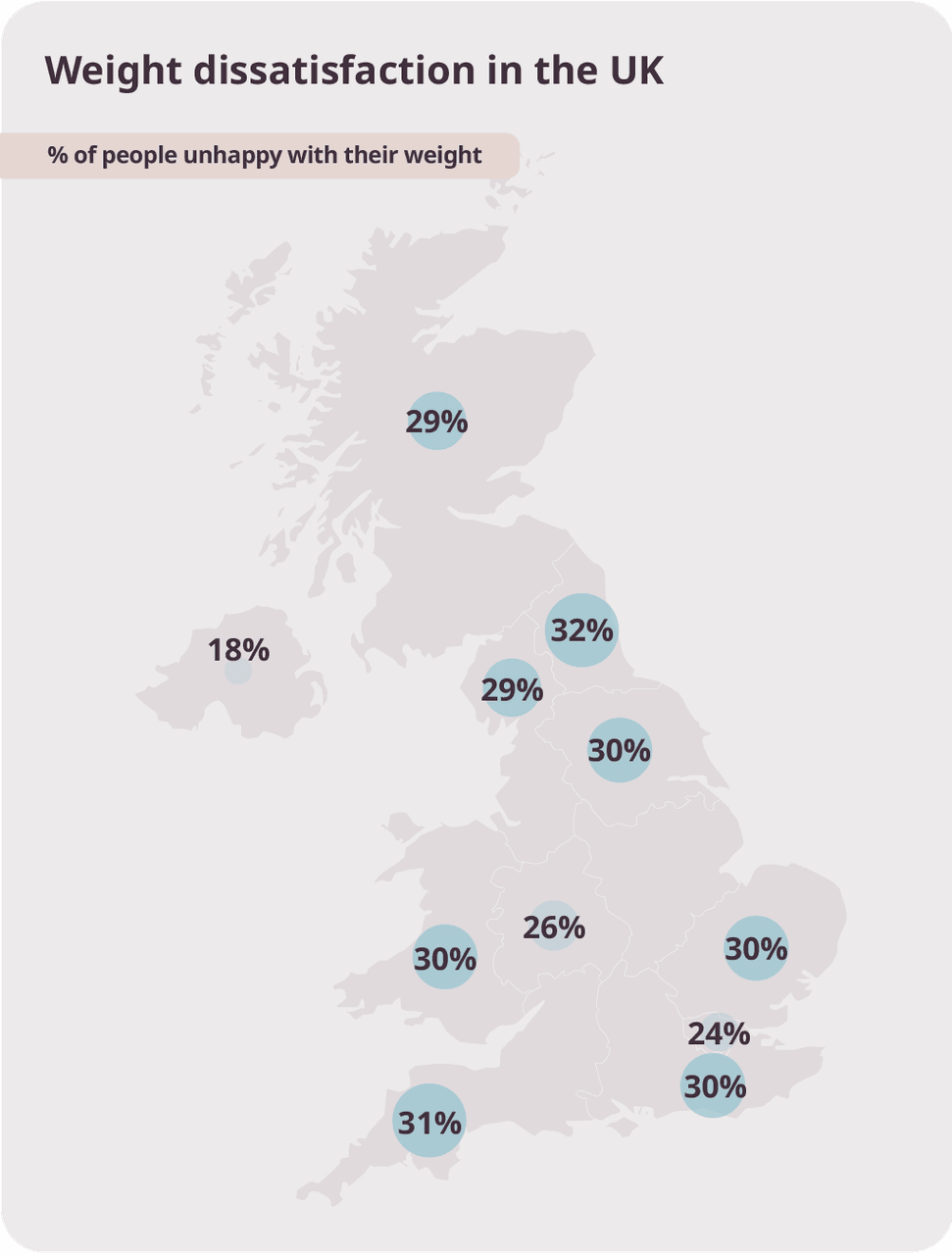
Feelings about weight vary widely across the UK. In the North East, almost one in three adults (32%) say they are unhappy with their weight, the highest of any region, followed closely by the South West (31%) and parts of England and Wales where around three in ten (30%) report dissatisfaction.
Rates are slightly lower in Scotland and the North West (29%), falling further in the West Midlands (26%) and London (24%). Northern Ireland reports the lowest levels of dissatisfaction, with fewer than one in five adults (18%) saying they are unhappy with their weight. These differences reflect how regional pressures, environments, and access to support shape not only weight, but how people feel about it.
"This data shows that weight loss in the UK today is shaped by far more than personal effort alone. How people experience their weight depends on where they live, their stage of life, their mental health, and the pressures they are under day to day. We see clear regional differences, we see confidence and satisfaction drop sharply in midlife and among parents, and we see how dissatisfaction with weight is becoming the norm rather than the exception.
“We're also seeing a shift in how people respond. Medically supported weight loss treatments are giving people access to options that simply did not exist before, particularly for those who have struggled for years without the right support. For many, this is the first time weight loss feels achievable, personalised, and grounded in healthcare rather than judgement."
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
What changed in 2025
By 2025, the shift to remote and hybrid working had settled in. Daily life looked different, with less built-in movement and blurred boundaries between work and rest. While people adapted with resilience, these changes quietly reshaped weight patterns across the UK, influencing how our bodies move, eat, and recover over time.
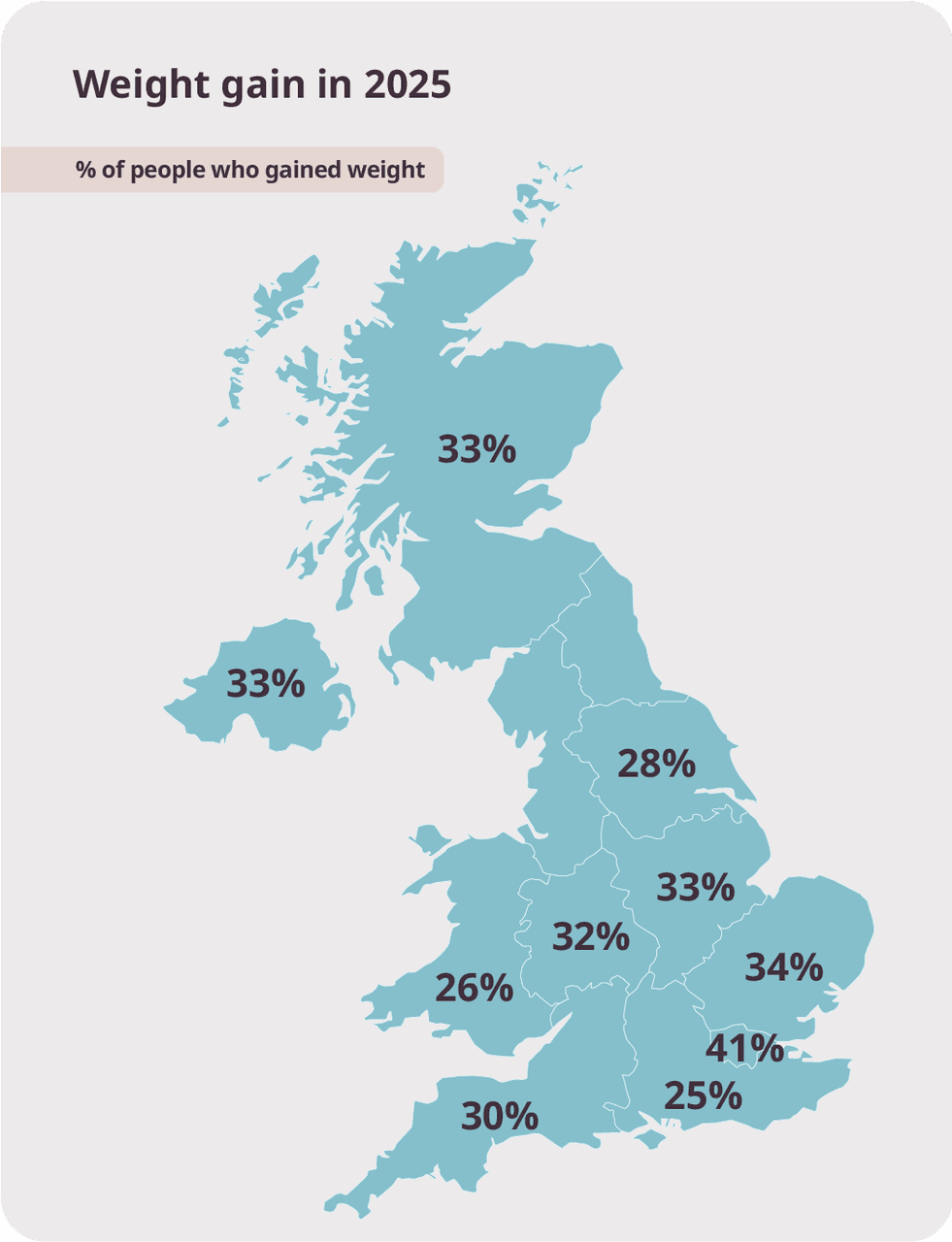
Weight change in 2025 was far from uniform. For many, things stayed the same. Around two in five adults (42%) reported no change to their weight. But for a significant share, the year tipped in the opposite direction, with almost one in three (32%) saying they had gained weight over the past 12 months.
Patterns varied by age and gender:
- Women were slightly more likely than men to report weight gain (33% compared with 31%).
- Younger adults stood out for different reasons. Those aged 18–34 were the most likely to have lost weight, with 29% reporting weight loss during the year.
Where people lived and how they worked made a clear difference:
- Greater London saw the highest levels of weight gain, with more than two in five adults (41%) putting on weight in 2025.
- Working from home also mattered. Nearly four in ten people (39%) working remotely reported weight gain, compared with 32% of those working on-site.
This difference reinforces how everyday routines continue to shape weight long after the initial shift to flexible working. With less built-in movement and blurred boundaries between work and rest, remote and hybrid patterns are still influencing how people eat, move, and manage their weight over time.
“The way people live and work has fundamentally changed, and weight patterns changed with it. Remote and hybrid routines removed a lot of everyday movement and blurred the boundaries between work, eating, and rest. Many people adapted well, but those small changes add up over time.
“What this data shows is that weight change follows routine, not willpower. This is why we focus so strongly on education around nutrition and movement, helping people understand how to adapt healthy habits to the realities of working from home, hybrid schedules, and modern life, rather than trying to force outdated routines to fit.”
Niya Mansuri, myBMI weight management and obesity expert
.png&w=3840&q=75)
Part 3: The impact of weight on mental wellbeing
Weight doesn’t just change bodies. It changes how people feel, think, and cope. It affects confidence, self-worth, anxiety, and resilience, shaping mental health every day, not just when the scale moves.
- One in three (30%) have seen some mental health improvements in 2025 but one in five (21%) saw theirs decline, rising if weight gain had occurred.
- Adults aged 45-54 saw the biggest declines in mental health with more than one in four (27%) reporting a decline.
- Single adults in the UK say the biggest declines in mental health (29%), whereas those who are married reported the biggest improvements (35%).
- Almost two in three (64%) current weight loss injection patients reported improvements to their mental health.
- More than half (51%) of those who have used, are using or have plans to use weight loss injections saw improvements in their mental health in 2025.
Mental wellbeing shifted in both directions in 2025. For some, things improved. Around one in three people (30%) reported better mental health over the year. But for many others, the opposite was true. One in five (21%) saw their mental health decline, with declines far more common among those who had gained weight, highlighting the close link between weight change and emotional wellbeing.
Midlife emerged as a clear pressure point:
- Adults aged 45–54 reported the steepest declines in mental health.
- More than one in four (27%) in this age group said their mental health worsened during the year.
This stage of life often brings overlapping pressures, from work and finances to caring responsibilities, and weight can amplify that strain rather than sit separately from it.
Connection and support also played a critical role:
- Single adults reported the highest levels of decline, with 29% saying their mental health worsened.
- Those who were married were most likely to see improvements, with more than one in three (35%) reporting better mental health in 2025.
This highlights the protective role that stability and support can play.
Medical support was linked to more positive outcomes:
- Almost two in three (64%) current weight loss injection patients reported improvements in their mental health.
- Looking more broadly, more than half (51%) of those who have used, are using, or plan to use weight loss injections saw mental wellbeing improve during 2025.
These findings underline that when people feel supported and see progress, the impact reaches far beyond weight alone.
“Weight has a constant presence in many people’s lives, not just physically, but mentally. It shapes confidence, self-worth, and how people cope with stress day to day. We see time and again that when weight feels out of control, mental wellbeing often suffers alongside it, particularly during high-pressure life stages or periods of isolation.
“We see education around the mental impact of weight as a crucial part of weight loss itself. Helping people understand what’s happening emotionally, as well as physically, allows them to approach change with more compassion, resilience, and balance. That’s what supports a healthier journey, both mentally and physically.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
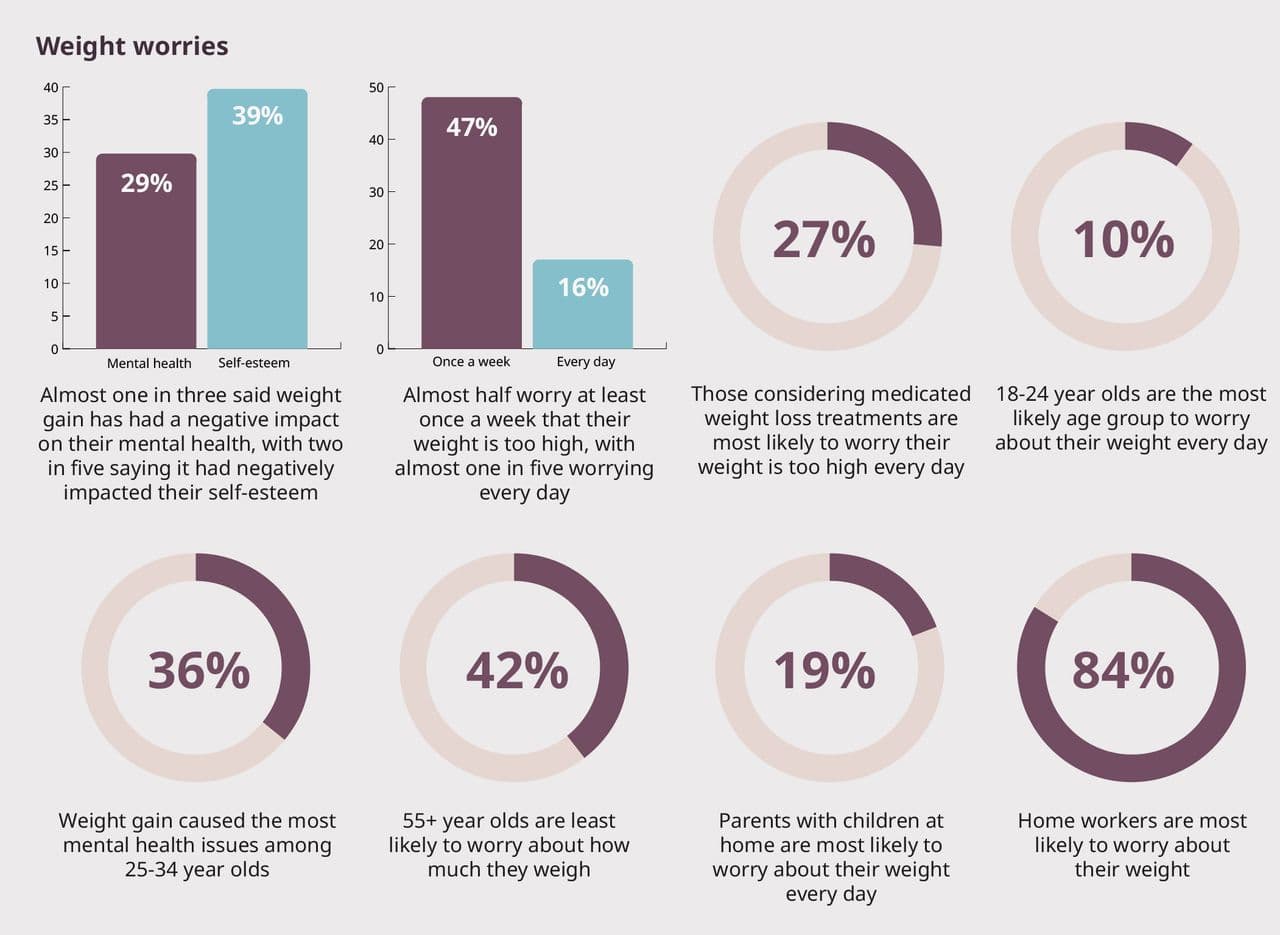
Weight worry is a constant presence for many people:
Almost one in three (29%) say weight gain has negatively affected their mental health, while two in five (39%) say it has damaged their self-esteem. And these concerns are not occasional.
Nearly half of adults (47%) worry at least once a week that their weight is too high, and almost one in five (16%) say they worry about it every day.
Daily weight worry is not evenly shared:
- People considering medicated weight loss are the most likely to worry daily, with more than one in four (27%) saying concerns about their weight are constant.
- Those aged 18–24 are the most likely age group to worry about their weight every day (10%).
The mental health impact of weight gain peaks slightly later:
- Among 25–34 year olds, more than one in three (36%) say weight gain has had a negative impact on their mental health.
Worry changes with age and responsibility, but it does not disappear:
- Adults aged 55+ are the least likely to worry about their weight, yet 42% still say it is a concern.
- Parents with children at home are more likely to worry about their weight every day (19%).
- Concern is especially high among those working from home, where an overwhelming 84% say they worry about their weight.
Weight worry is not fleeting or superficial. It is persistent, shaped by life stage, responsibility, and routine.
“Weight worry is something many people carry quietly. It’s there in the background, shaping confidence, self-esteem, and how people feel about themselves long before it becomes a medical issue. We see that this worry is often tied to life stage, responsibility, and daily routine, whether that’s parenting, working from home, or navigating early adulthood.
“At myBMI, we believe it’s essential to acknowledge and address this mental load as part of weight management. Helping people understand and normalise these worries allows them to approach change without shame and more clarity.”
Niya Mansuri, myBMI weight management and obesity expert
Improving nutrition feels overwhelming for many
Trying to eat better is not always experienced as empowering. More than one in three adults (37%) say they agree that improving their nutrition feels overwhelming, including 11% who strongly agree. A further 26% somewhat agree, showing that for a significant proportion of people, better nutrition feels difficult to manage rather than straightforward.
“When people say nutrition feels overwhelming, often it’s because the information feels confusing, conflicting, or difficult to apply to real life. There’s a lot of pressure to ‘get it right’, which can make even small changes feel daunting. Through our advice, we aim to help patients understand nutrition in a clear, practical way, so it feels manageable rather than intimidating. When people know what matters for them, nutrition becomes something they can work with, not something that feels out of reach.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
The negative impact of weight on real life
Weight gain does not stay contained to health or appearance. It spills into everyday life, shaping how people show up at work, in social situations, and in how they see themselves. Confidence, self-worth, and comfort in daily interactions are often among the first things to be affected.
Putting on weight changes how people see themselves and how they move through the world. These impacts are felt across confidence, work, and social life, shaping everyday behaviour rather than isolated moments.
Confidence and self-esteem are widely affected:
- Two in five adults say weight gain has damaged their self-esteem.
- For half of adults, weight gain has knocked their confidence more broadly.
These are not abstract feelings. They show up in everyday moments, conversations, decisions, and how visible people feel comfortable being.
The impact extends into working life:
- Almost one in three (27%) say gaining weight has made them feel less confident in the workplace.
- This loss of confidence is felt most strongly among millennials, where 33% say weight gain has affected how confident they feel at work.
Social confidence is also affected:
- More than two in five people (41%) say putting on weight has made them feel less confident in social settings.
- Weight gain increases exposure to negative experiences with diet culture. One in three (31%) say putting on weight made them more likely to have a negative experience with dieting.
Our data shows that weight gain does not just change bodies. It reshapes confidence, behaviour, and everyday experience.
“What people often don’t expect is how quickly weight gain starts to affect everyday life. It’s not just about how someone looks, but how confident they feel speaking up at work, showing up socially, or even being seen. We hear from patients that weight can shape behaviour, from avoiding situations to feeling more exposed to judgement or diet culture. We recognise that these real-life impacts are just as important as the physical ones. Addressing confidence, self-worth, and lived experience is a crucial part of supporting healthier, more sustainable change."
Niya Mansuri, myBMI weight management and obesity expert
.jpg&w=3840&q=75)
The hidden impact of weight gain
“What we’re seeing is that weight gain rarely affects the body alone. It impacts confidence, mental health, work, and social life, often at the same time. For many people, the worry becomes constant, especially when weight change feels out of their control. That’s why access to the right support matters. When people feel supported and see progress, the impact on mental wellbeing can be just as significant as the physical change.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Part 4: The heavy pressures of everyday life
Rising living costs, long working hours, stress, and limited time are making healthy choices harder to maintain, even for people who are motivated and trying to do the right thing. For many, the challenge is not knowing what a healthy lifestyle looks like, but being able to afford and maintain it day after day.
“One of the most concerning findings from our research is that one in three (32%) people say they are not able to consistently eat healthily in their everyday lives, and this rises to almost half (44%) of 18–24 year olds.
“When less nutritious, ultra-processed foods are often cheaper, more convenient, and more readily available than fresh fruit and vegetables, the odds are stacked against people. Add limited healthy options at work or when socialising, and it becomes clear that cost, not lack of motivation, is a major driver of the UK’s ongoing struggle with obesity.”
Niya Mansuri, myBMI weight management and obesity expert
Food finances
Cost is one of the most persistent pressures shaping weight in the UK. Rising food prices are not just influencing what people buy, but how realistic it feels to maintain healthier habits over time. When cheaper options consistently undercut nutritious ones, cost becomes a deciding factor, even for those who are motivated to make better choices.
- More than 34% of people say that healthier options costing more unhealthy foods like Ultra Processed Foods (UPFs) have negatively affected their weight.
- Cheaper, less nutritious foods negatively affected the weight of 42% of 18–24 year olds in 2025.
Where cost hits hardest
Cost pressure is not felt evenly. It hits hardest among groups already managing competing demands on time, money, and energy.
- Lower-income households, where healthier food is more likely to be seen as unaffordable or difficult to prioritise.
- Families with dependent children, where food budgets must stretch further to cover more mouths.
- Midlife adults, who are often balancing rising household costs alongside work and time pressure.
Cost pressure does not disappear in higher-income groups, but its impact is softened. These respondents are more likely to describe food costs as neutral rather than negative, suggesting greater flexibility rather than an absence of pressure.
- 34% say the cost of healthy food negatively affects their weight.
- Cost pressure increases consistently as household income decreases.
Food cost is not a niche concern. It is a sliding pressure that intensifies as income falls, shaping weight outcomes long before individual choice comes into play.
“Cost is one of the most powerful forces shaping weight, and it rarely acts alone. We see it hit hardest when people are already juggling family responsibilities, work pressure, and limited time. For many households, healthier food isn’t rejected, it’s deprioritised because budgets have to stretch. Even in higher-income groups, cost pressure doesn’t disappear, it just becomes easier to absorb. We understand that weight loss journeys have to factor in cost at every stage. Support only works when it’s realistic, affordable, and designed to fit the pressures people are already living with.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Work and social pressures impact how we put on weight
How we work, where we eat, and how we socialise all influence the choices available to us, often making healthier habits harder to sustain, even with the best intentions.
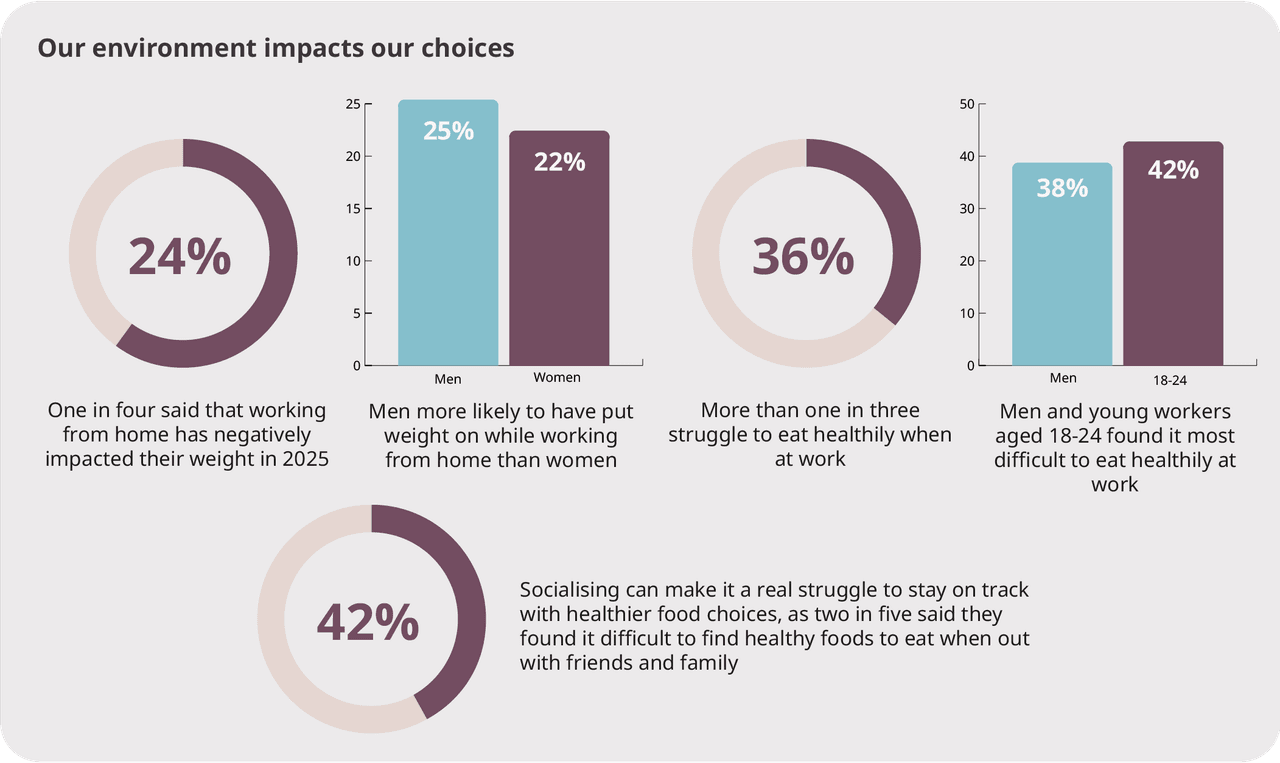
Working patterns continue to influence weight.
- One in four (24%) people say working from home has negatively impacted their weight.
- Men are more likely to report weight gain while working remotely (25%) compared with women (22%).
- This suggests home working continues to reshape eating and movement patterns in different ways.
The workplace presents its own challenges.
More than one in three people (36%) say they struggle to eat healthily when at work.
This difficulty is most pronounced among:
- Men (38%)
- Younger workers aged 18–24, where more than two in five (42%) report struggling
Social life adds further pressure.
- More than two in five people (42%) say they find it difficult to find healthy food options when socialising with friends and family.
- Social environments often prioritise convenience and indulgence over nutrition.
Weight gain is rarely about isolated choices. It is shaped by the demands and expectations of work and social life, played out day after day.
“What this data reflects is how much our environments shape our habits, often without us realising. Working from home, eating on the go, and socialising around food all change what choices are available in the moment. Even people with the best intentions can find it harder to eat well when convenience takes over. We focus on helping people adapt nutrition and movement to the realities of work and social life, rather than expecting willpower to overcome environments that are working against them.”
Niya Mansuri, myBMI weight management and obesity expert
Part 5: The barriers to healthy lifestyle choices
Most people know what a healthier lifestyle looks like. The challenge is not motivation, but reality. Daily pressures, cost, convenience, and environment often work against even the best intentions, making healthy choices harder to sustain over time.
Intentions to eat better are clear:
Avoiding junk food is now the top weight management priority for adults in the UK, with 44% saying it is their main focus.
- 40% are prioritising portion control.
- 27% say eating more whole foods is a key goal.
This shows a strong desire to improve diet and nutrition, driven by growing awareness of the impact of high-calorie, low-nutrition foods.
However, intention does not always translate into action
Despite strong motivation, adults across the UK face consistent barriers that make healthy lifestyle choices harder to maintain.
The most common factors negatively affecting weight and the ability to maintain a healthy lifestyle are:
- Easy availability of takeaway and junk food options (38%)
- Cost of healthier foods like fruit and vegetables compared with cheaper, poor-nutrition options such as ultra-processed foods (34%)
- Supermarket promotions like BOGOF offers on poor-nutrition foods (31%)
- Working from home, reducing routine movement and changing eating patterns (24%)
- Limited access to local sports and workout facilities (15%)
Healthy choices are often competing against systems designed for convenience and cost, not long-term wellbeing.
“The challenge isn’t motivation, it’s trying to maintain healthy choices in environments that constantly push us in the opposite direction. Cost, convenience, promotions, and daily routines all add friction, even when intentions are strong. We recognise these barriers and that lasting change means working through them, not ignoring them.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Nutrition
Eating well is often presented as a simple choice, but the reality is more complicated. The cost of nutritious food, where people live, and what is readily available all play a role in shaping diets. For many, access to healthy nutrition is uneven, influenced by income, and the options available at work or when socialising, making consistency harder to achieve.
Easy access to takeaway and junk food undermines good intentions
Across the UK, two in five people (38%) say that having takeaway and junk food readily available near them has a negative impact on their weight. For many, temptation is not occasional. It is built into daily routines, neighbourhoods, and work patterns.
This pressure is felt most strongly among:
Younger adults, who are more likely to live in areas with a high density of takeaway outlets
- 44% of 18–24 year olds
- 43% of millennials
People in relationships, where shared routines and social eating can make healthier choices harder to maintain
- 46% report a negative impact
Workers, particularly those spending time on-site
- 42% of on-site workers vs 39% of people working from home
It is also more pronounced among urban residents, where food delivery apps, late-night options, and high street takeaways make less nutritious food the easiest and most visible choice.
The influence of takeaway and junk food also shifts for those exploring medical support.
Among people considering weight loss injections but not yet using them, 45% say easy access to takeaway and junk food has a negative impact on their weight. This falls to 39% among those who have used the treatment in the past, suggesting that medically supported weight loss can help reduce the pull of less nutritious options. For many, this points to a reset in how food choices are experienced, making healthier decisions feel more manageable over time.
“Eating well is rarely about knowing what’s healthy. Most people already do. The challenge is living in an environment where less nutritious food is cheaper, easier to access, and constantly visible. When takeaway and junk food are built into daily routines, resisting them takes effort every single day.
“We see nutrition as something that has to work within real life. Through education, practical guidance, and, where appropriate, medical support, we help people reduce the constant pull of less healthy options so that better choices feel more achievable and less exhausting over time.”
Niya Mansuri, myBMI weight management and obesity expert
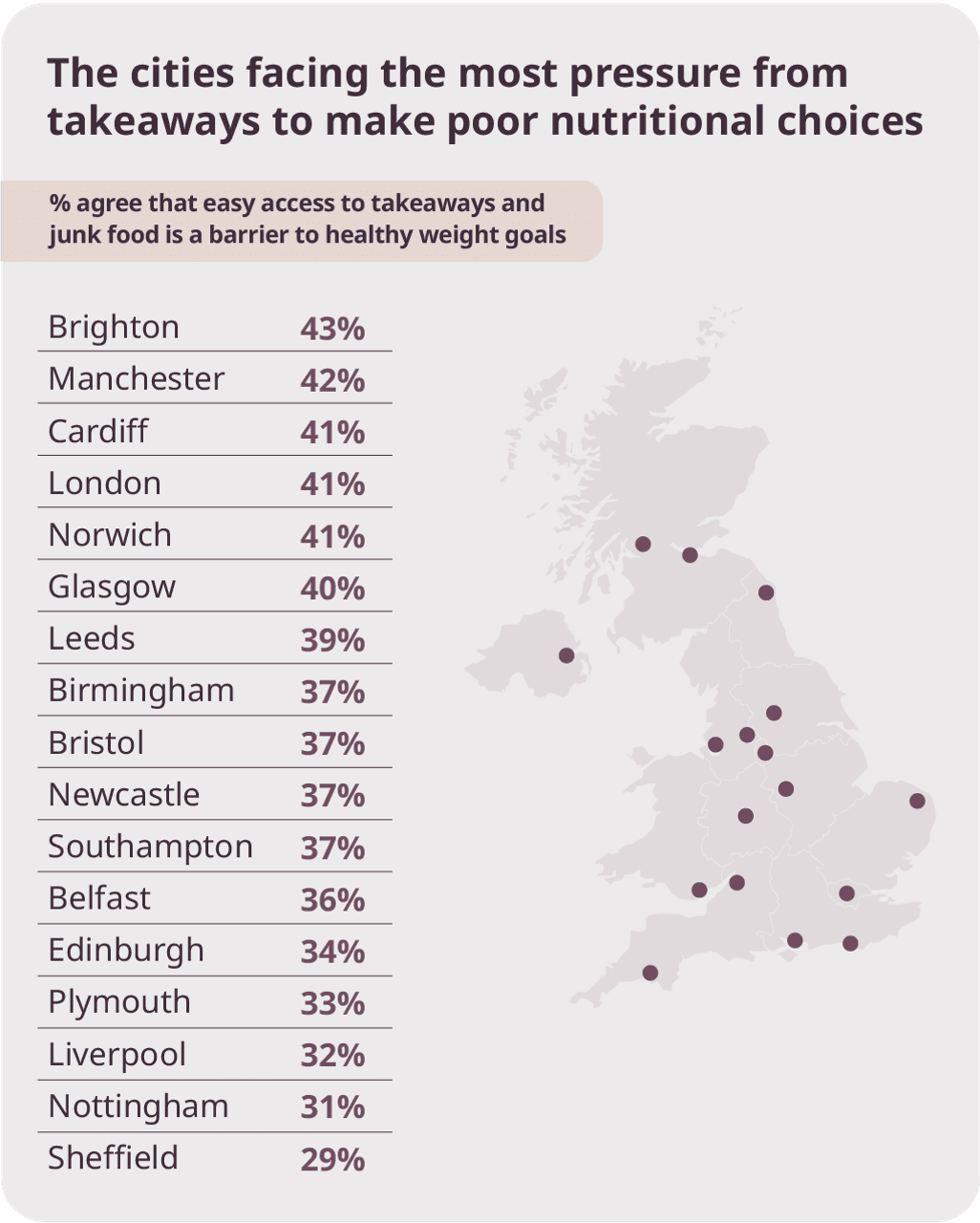
Access to takeaway and junk food remains one of the biggest barriers to healthy eating across UK cities. In Brighton, 43% of adults say it negatively affects their weight, followed by Manchester (42%) and Cardiff, London, and Norwich (all 41%). Across most major cities, around four in ten adults report a similar impact, showing how widespread this pressure has become.
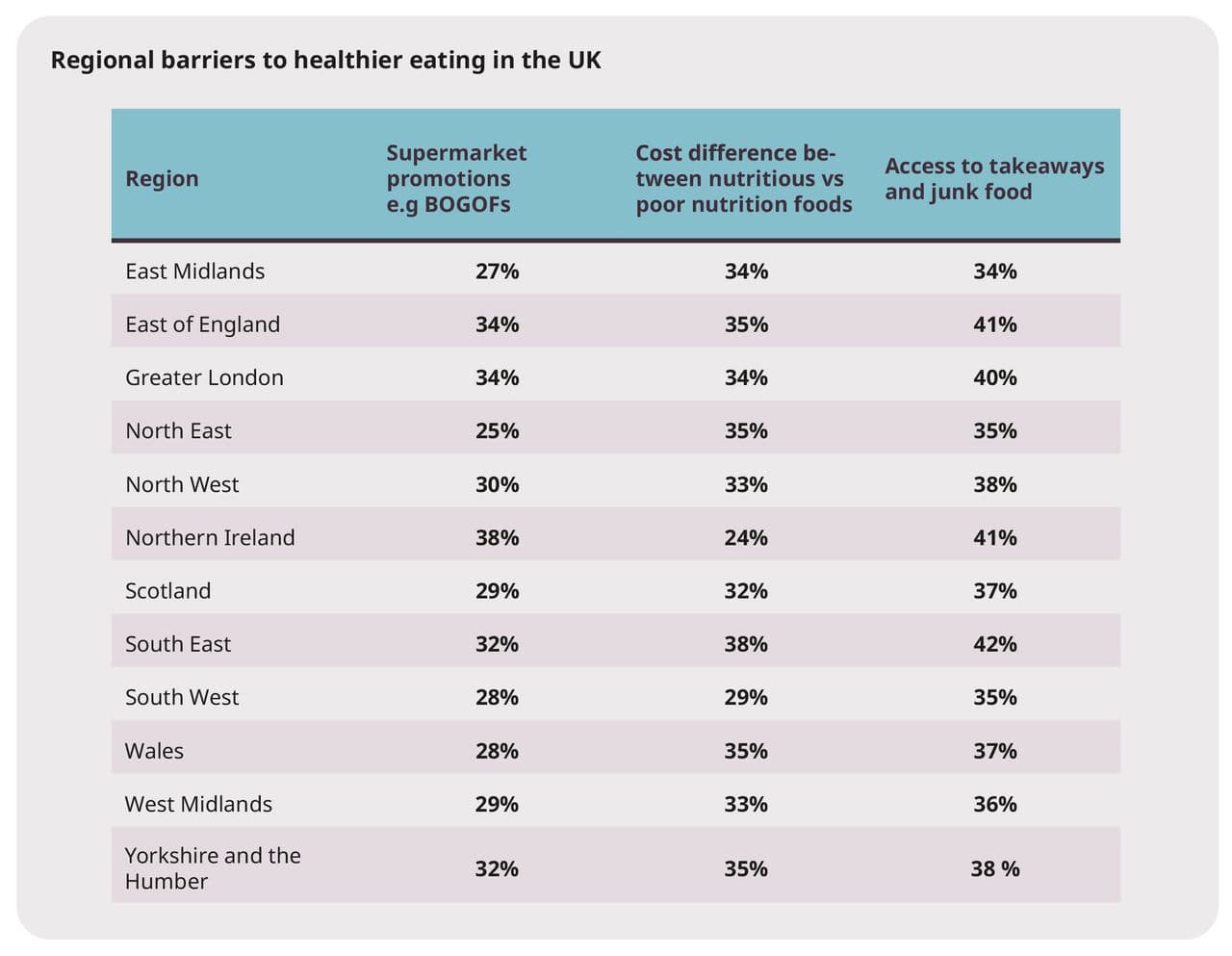
This pattern holds at a regional level. In 11 out of 12 UK regions, access to takeaway and junk food is the single biggest factor undermining healthy lifestyle choices, with the strongest impact seen in the South East (42%). For most urban residents, availability is the primary challenge. The exception is a handful of cities, including Brighton, Liverpool, Nottingham, Sheffield, and Southampton, where the cost of healthy food outweighs access as the greater barrier.
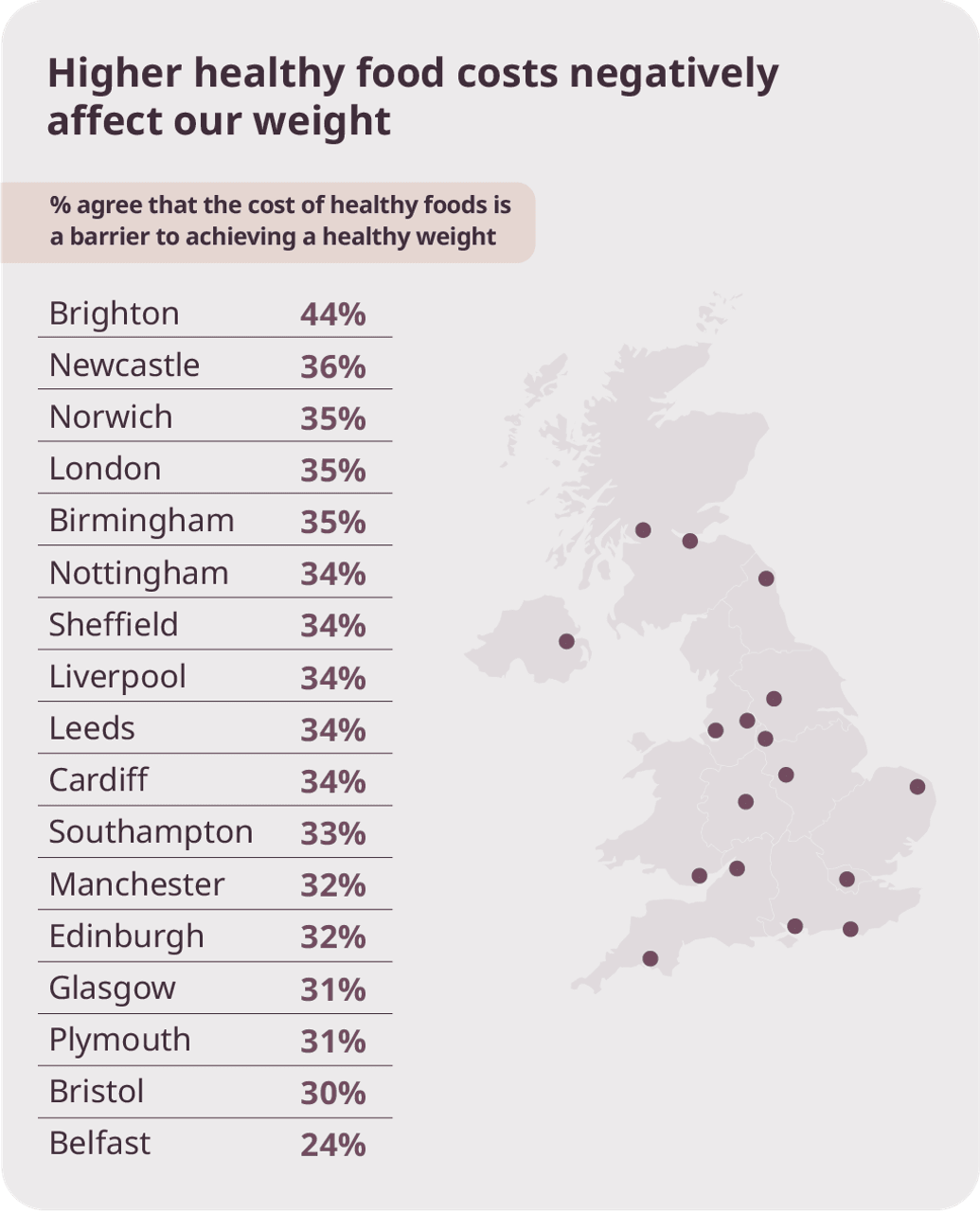
Food cost is a major barrier to healthy lifestyle choices
Cost remains one of the strongest forces shaping how people eat. The higher price of nutritious foods, combined with supermarket promotions that favour cheaper, less healthy options, continues to undermine even the best intentions.
The cost gap matters:
- 34% of adults say the price difference between healthier foods and cheaper, less nutritious options is a major barrier to eating well.
- Supermarket promotions such as BOGOF deals on poor-nutrition foods further tilt choices away from healthier options.
Younger adults feel the pressure most:
- Among 18–24 year olds, two in five (40%) say cost pushes them towards less healthy food choices.
- Lower incomes and tighter budgets mean price often outweighs nutritional value at this life stage.
Regional and city-level impact:
- In the North East, the region with the highest obesity rates in the UK, 35% say the higher cost of healthy food is the single biggest barrier to a healthy lifestyle,
- Brighton reports the highest city-level impact, with 43% saying the cost of healthy food negatively affects their weight.
Cost versus other pressures:
In cities such as Bristol (30%) and Leeds (34%), cost remains a top barrier but sits alongside:
- Easy access to junk food
- Supermarket promotions on poor-nutrition foods
This shows how pricing, promotions, and affordability continue to shape everyday food choices, often pushing people away from healthier options despite strong motivation to eat well.
“Cost is one of the biggest factors shaping how people eat. We see that many patients want to make healthier choices, but when nutritious food costs more and promotions consistently favour less healthy options, those choices become harder to justify week after week. This pressure is felt most by younger adults and families, but it affects people across the UK.
“Weight management has to account for affordability as well as nutrition. Supporting people means helping them make better choices within real budgets, not expecting cost to be something they can simply ignore.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Supermarket promotions actively work against healthy choices
Supermarket promotions are not neutral. For many people, they actively shape what ends up in the trolley, often nudging choices towards cheaper, less nutritious foods rather than healthier options.
Almost one in three adults (31%) say BOGOF deals or promotional offers on unhealthy foods have a negative impact on their weight. In contrast, just 6% say these offers have a positive effect, highlighting how rarely promotions support healthier eating.
These promotions are especially influential for certain groups:
Lower-income households, where stretching budgets matters most
- One in four (25%) adults earning £15k or less say BOGOF offers make it harder to eat healthily.
Families, where promotions often guide weekly food shops
- 35% of parents with young children at home say supermarket offers are a barrier to healthier choices.
Younger shoppers, who are more likely to be earning less and actively looking for bargains
- 38% of Generation Z shoppers struggle with this barrier, compared with 24% of Baby Boomers, who are least affected.
This shows how supermarket pricing strategies can quietly undermine healthy intentions, particularly for those under the greatest financial pressure, turning affordability into a powerful driver of poorer nutrition.
“Our everyday food environments can undermine even well-intentioned efforts to eat better. People are surrounded by promotions that reward bulk buying of low-nutrition foods, while healthier options are often more expensive, less visible, and harder to prioritise. Over time, this shapes habits, not because people lack understanding or motivation, but because unhealthy choices are made the easiest and most affordable option. For many, particularly families, younger adults, and those under financial pressure, eating well means constantly pushing back against how food is priced and promoted.”
Niya Mansuri, myBMI weight management and obesity expert
.png&w=3840&q=75)
Nutrition barriers for families
For families with dependent children, healthy eating is shaped by a stack of everyday pressures that make consistency harder to maintain, even when motivation is high.
Families are more likely to say that cost, convenience, and supermarket promotions actively work against healthier choices. Larger food shops, tighter budgets, time pressure, and the need to prioritise value all play a role. Parents are navigating the same food environment as everyone else, but with far less flexibility to absorb rising costs or avoid constant exposure to less healthy options.
Compared with adults without children at home, families are more likely to face nutrition barriers at higher-than-average levels:
- 34% say the cost of healthy food negatively impacts their weight
- 38% say easy access to takeaway food negatively impacts their weight
- 31% say promotions on unhealthy foods undermine their progress
Family life amplifies the pressures already present in the wider food environment, making healthy eating harder to maintain over time, not through lack of effort, but through cumulative constraint.
“Families are not failing at healthy eating. They are operating under far more pressure. When you are feeding more people, managing tight budgets, juggling work and childcare, and shopping in environments designed around convenience and promotions, consistency becomes the hardest part. We see parents trying to make the best choices they can, but with fewer margins for error. Family life changes what ‘healthy eating’ realistically looks like, and support has to reflect that."
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Nutrition barriers: injection users comparison
Comparing those who use weight loss injections with those who do not shows how treatment can change not just outcomes on the scale, but how manageable everyday food choices feel. Barriers do not disappear, but for many they are experienced differently, with less pull, less pressure, and greater control over decision-making.

People using weight loss injections are navigating the same food environment as everyone else. Cost pressures, convenience, and access do not disappear. The difference is how those pressures are experienced and managed.
Medical support changes the balance, not the reality:
- Injection users still face cost and access barriers, but they are better equipped to manage them.
- Treatment appears to reduce the impact of environmental pressures, rather than remove them altogether.
Without support, barriers have more pull:
- Non-users are more likely to be pulled off course by convenience, promotions, and price.
- Injection use is linked to greater intentionality, not perfect conditions.
What our data shows:
- Almost two in five (38%) say takeaway availability negatively impacts their weight, but this effect is weaker among injection users.
- 31% say unhealthy food promotions undermine progress, with the impact felt more strongly by non-users.
- 16% say they are not doing anything specific to manage their diet, a pattern more common among people not using weight loss injections.
- People who are using or planning to use injections are more likely to be actively changing what they eat, rather than relying on medication alone.
- Injection users are more likely to prioritise avoidance, portion control, and structured approaches to eating.
The takeaway
Weight loss injections do not remove barriers, but they help people regain control in an environment that otherwise works against them.
“Food choices don’t happen in a vacuum. They’re shaped by busy days, work patterns, family life, and stress. People working from home or juggling multiple responsibilities often describe eating as reactive rather than planned. Parents are more likely to make choices based on cost and convenience, while single adults are more influenced by what’s readily available or tempting in the moment.
What matters is not getting it right all the time, but being able to make healthier choices when you can, with the right support around you.”
Niya Mansuri, myBMI weight management and obesity expert
Movement
Most people know that moving more is good for them. But staying active is not equally easy for everyone. Time, energy, confidence, health, money, and caring responsibilities all shape how realistic movement feels in everyday life. For many, the barrier is not a lack of motivation, but trying to fit activity into lives that already feel full.
Movement is happening, but it is constrained
At a national level, most people are doing some exercise, but not always in the way or at the level they would like.
Age makes a clear difference:
- Among 18–24 year olds, one in five (18%) say they do not exercise.
- Among those aged 55+, this rises sharply to more than one in three (34%).
- Millennials are the most active generation, exercising for 5 hours a week, an hour more than the national average.
- Average weekly exercise falls from 5 hours in younger adults to 4 hours among those aged 55+.
Where and how people work also shapes movement:
- Londoners are the most active, exercising for an average of 5 hours per week across all ages.
- Adults in the East Midlands report the lowest average exercise time, at under 4 hours per week.
- Adults who work from home exercise for around 5 hours a week, 1 hour more than those who go into the office (4 hours).
This is not simply about motivation. It reflects health limitations, confidence, and fear of injury increasing with age, alongside routines that either support or restrict everyday movement.
“Moving more is often described as the easy part of looking after your health, but for many people it’s one of the hardest. Whether someone feels able to be active depends on things like their job, their health, whether they’re caring for children or others, how tired they feel, and how confident they are in their own body. What we see in the data is that people aren’t lacking motivation. They’re trying to make movement fit around busy, demanding lives. Supporting people to move in ways that feel realistic and manageable is far more important than telling them they should be doing more.”
Ayesha Bashir, Obesity Expert and Prescribing Pharmacist
Income shapes capacity, not intent
Income level makes a clear difference to how much movement feels possible, not how much people care about being active.
- Lower-income adults are significantly more likely to sit in the “cannot exercise” category, with 42% saying they are unable to exercise.
- Those earning under £15k average 3 hours of exercise per week, 1 hour below the national average.
Higher-income adults are far more likely to reach higher activity levels.
- 25% of higher earners reach 6+ hours of exercise per week.
- Fewer than one in ten (9%) low-income adults are able to do the same.
Parents move differently, not less.
Parenthood reshapes how and when movement happens.
- Parents with young children at home average 5 hours of exercise per week.
- Adults without children average 4 hours.
- Parents with adult children still living at home exercise the least.
For many parents, movement is incidental rather than planned. It’s fitted in around childcare, work, and household responsibilities, squeezed into daily life rather than prioritised as dedicated exercise.
Confidence and fear of judgement are major barriers to movement.
The challenge is not knowing that exercise is beneficial but feeling comfortable enough to do it.
- One in five (19%) say low confidence in their body is a barrier to exercising regularly.
- Almost one in five (18%) say fear of judgement keeps them home and moving less.
Younger adults struggle most with confidence:
- Adults aged 18–24 (29%) and 25–34 (29%) are the most likely to say confidence is a barrier.
- This drops among 45–54 year olds, where 20% report confidence issues.
Relationship status makes a difference:
- Single adults are less confident (22%) and more likely to fear judgement (24%).
- Those in a relationship report slightly higher confidence (20%) and lower fear of judgement (21%).
Parenthood amplifies confidence barriers:
- Parents with young children are significantly less confident, with 27% reporting confidence as a barrier.
- This compares with 19% among adults without children.
Confidence gaps are widest around medical weight loss:
- People using weight loss injections are more likely to struggle with confidence (29%) and fear judgement (28%).
- Those not considering medical treatment are much less likely to struggle with confidence (14%) and are far less likely to fear judgement (12%) when exercising in public.
Movement barriers are as much emotional and social as they are physical, shaped by confidence, visibility, and how safe people feel being active around others.
“Movement is one of our core pillars because we know it isn’t a one-size-fits-all behaviour. Confidence, fear of judgement, time, and life stage all shape whether someone feels able to move at all. That’s why we support movement in ways that feel realistic, gradual, and personal, not performative or punishing. For many people, especially those navigating weight loss, feeling safe and supported to move is just as important as the movement itself.”
Niya Mansuri, myBMI weight management and obesity expert
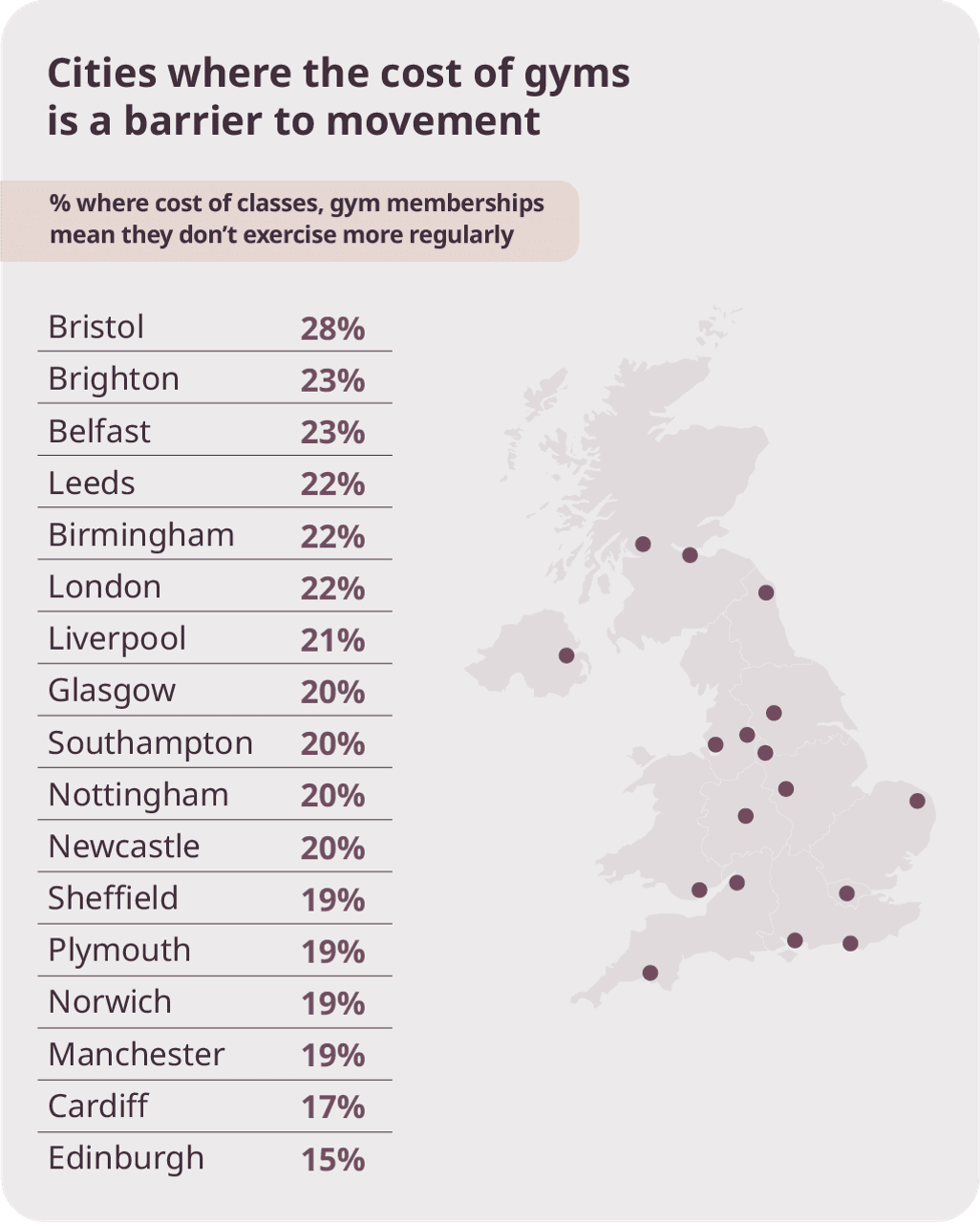
Cost is a major barrier to moving more
For many adults, the price of gyms and classes shapes whether increasing activity feels possible.
- One in five (21%) say the cost of gym memberships and classes is a barrier to proactively increasing movement.
- This rises to one in four (26%) among Gen Z.
Working patterns shape how cost is experienced:
- Cost is the biggest barrier for people who work from home, with 26% reporting this compared with 21% overall.
- Those who work on-site are more likely to feel they already do enough exercise, with 30% saying they do not need to go to the gym.
Household circumstances make a clear difference:
- Low-income adults are the least likely (19%) of any income bracket to say gym costs are a barrier, viewing gym membership as a necessary choice.
- Parents with young children at home are more likely to struggle with this additional household bill, with 27% reporting cost as a barrier.
The cost of fitness is a barrier to weight loss
For many adults, the price of the fitness industry has quietly pushed paid-for movement out of reach. While motivation exists, cost limits access to the structure, accountability, and community that can make activity easier to sustain.
This shows how widespread disengagement from paid fitness has become, even as movement remains a stated priority.
Who does invest, and how, varies by gender and age:
- Men are more likely to invest in a monthly gym membership (47% vs 30% of women).
- Women are more likely to pay for fitness classes (49% vs 41% of men).
Younger adults engage differently:
- 18–24 year olds are the most likely to pay for a fitness app or subscription (69%).
- 25–34 year olds are the most likely to pay for a gym membership (76%) or fitness classes (65%).
Cost does not remove interest in fitness, but it does reshape how people participate. For many, paid fitness is no longer a default option, limiting access to the motivation, structure, and social support that can help turn intention into long-term change.
“These findings show that cost is not dampening interest in fitness, but it is changing how people engage with it. When paid-for movement becomes out of reach, many lose access to the structure and support that help habits stick. Weight management support should fit into everyday life, not expect gym memberships or expensive classes."
Niya Mansuri, myBMI weight management and obesity expert
Movement looks different for people using weight loss injections.
Those using, or planning to use, weight loss injections report a more active relationship with movement compared with non-users.
Compared with people who have never used weight loss injections, injection users are:
- Less likely to say they cannot exercise (13% vs 28%).
- More likely to reach 6+ hours of exercise per week (27% vs 14%).
Activity levels also increase after starting treatment:
- Before using weight loss injections, average weekly exercise sat at 4 hours.
- Once injections are started, this increases to 5 hours per week.
Medical weight loss support may help make movement feel more achievable. Rather than replacing exercise, treatment appears to support confidence, energy, and consistency, helping people engage more with movement in ways that fit into their everyday lives.
Movement in 2026
The challenge with movement is not awareness. It is sustainability.
Most people know they should move more, and many already do some form of activity. The problem is not getting started. It is staying consistent when life gets busy, energy dips, confidence wavers, or progress feels slow. Over time, confidence, consistency, and progression are the first things to break down under real-world pressure.
Movement becomes harder to sustain when it feels all-or-nothing, when low-effort activity feels like it “doesn’t count”, or when fear of injury, judgement, or failure creeps in. Without the right support, people stop tracking progress, then stop prioritising movement altogether.
In 2026, supporting movement means rethinking what success looks like. It means:
- Reducing fear of failure or injury, especially among those returning to movement.
- Validating low-intensity and incidental movement as meaningful, not lesser.
- Making progress visible, realistic, and achievable over time.
- Supporting confidence and consistency, not just targets or step counts.
“People don’t stop moving because they don’t care. They stop because movement starts to feel too hard, too punishing, or like it’s not making a difference. What we see at myBMI is that when effort feels achievable and progress feels rewarding, people keep going. When it feels unrealistic or demoralising, they disengage. Supporting movement means meeting people where they are, not where we think they should be.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
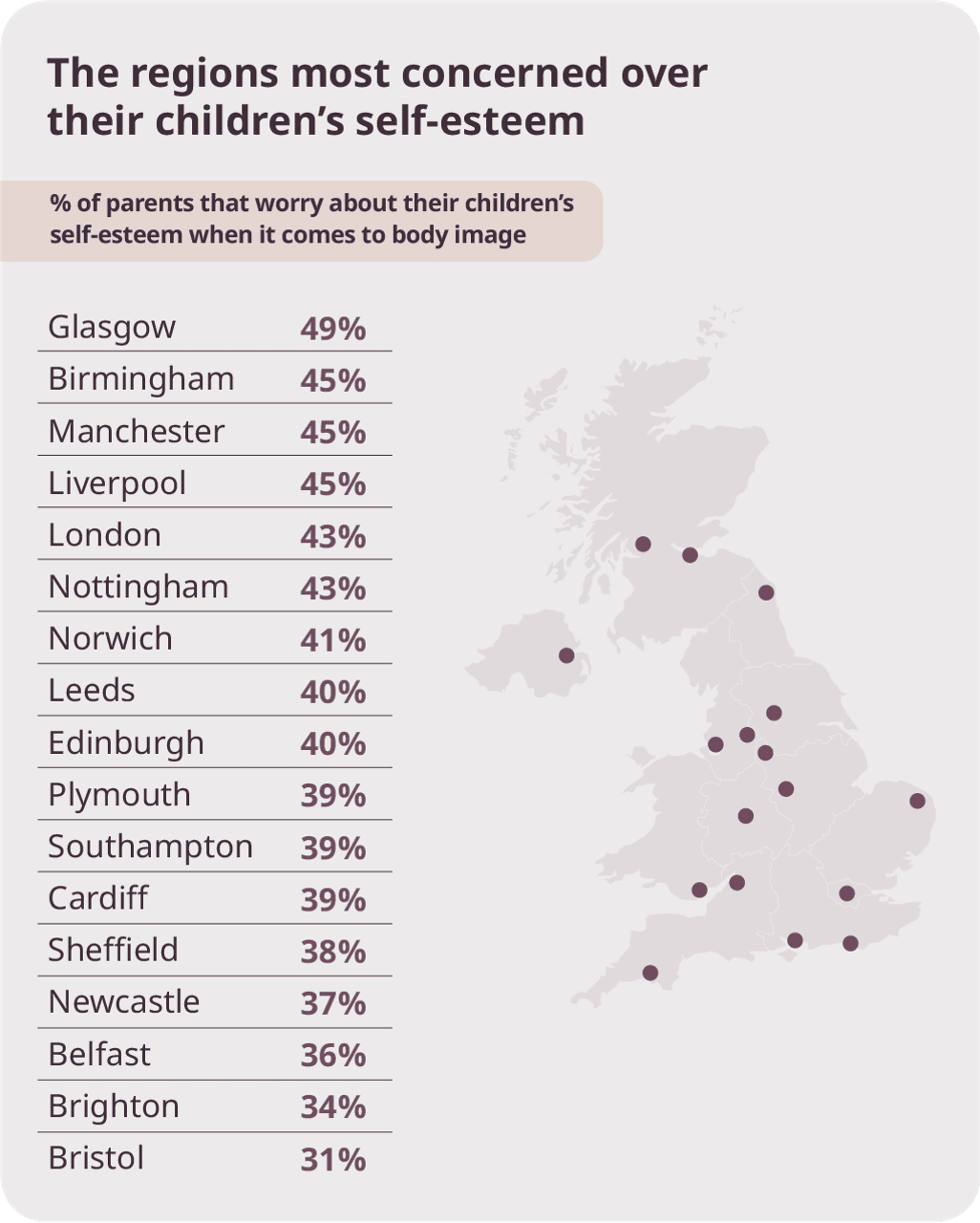
Part 6: Our impact on the next generation
Attitudes to weight are being shaped earlier and more intensely than ever before. Social media, filters, AI-generated content, and diet culture are influencing how young people see their bodies, food, and self-worth, often long before health behaviours are fully formed. How we respond now will shape the confidence, wellbeing, and relationship with weight of the next generation.
Diet Culture
Diet culture is not new, but its impact is becoming harder to ignore. Built on judgement, unrealistic standards, and constant scrutiny, it shapes how people think about food, bodies, and self-worth. For many, it has become louder, more persistent, and more damaging over time.
A majority of the UK believes diet culture has worsened:
More than 55% of UK adults say diet culture has become significantly more harmful during their lifetime.
Women are more likely to feel this impact (58%) than men (53%).
Generational experience shapes perception:
- Baby Boomers are the most likely to say diet culture has worsened (61%), having lived through decades of shifting pressure, from the “keep fit” eras of the 1970s and 1980s, to judgemental tabloid culture in the 1990s, and the rise of unsolicited advice and comparison on social media since the early 2000s.
- Despite having lived through a much shorter timeframe, almost half of Gen Z (49%) say diet culture has already become more harmful during their lifetime.
When weight management meets diet culture:
People using weight loss injections are more likely to say diet culture has worsened (56%) compared with non-users (51%). This suggests that increased engagement with weight management can bring greater exposure to diet culture, comparison, and weight-focused messaging, rather than reducing it.
Attitudes and self-esteem:
- One in four (24%) said their own attitudes to their own bodies have negatively influenced their children’s views on weight. Men (26%) are more likely to feel this than women (22%).
- Two in five parents worry about their children’s self-esteem around body image.
“These findings underline how early, and how powerfully, attitudes to weight are now being shaped. Young people are growing up surrounded by diet culture, social media, and constant comparison, often before they have the tools to understand health in a balanced way. That pressure does not disappear in adulthood and, for some, greater engagement with weight management can actually increase exposure to judgement and stigma rather than reduce it.
There is a clear responsibility to respond differently. Education, open conversations, and tackling stigma need to sit alongside access to safe and effective weight management support. Supporting people’s health should never come at the cost of self-worth, and how we approach weight today will shape not only individual outcomes, but the confidence and wellbeing of the next generation.”
Niya Mansuri, myBMI weight management and obesity expert
Social media
Social media has become a constant backdrop to how bodies are seen, compared, and judged. Filters, edited images, and algorithm-driven content shape expectations around appearance, often blurring the line between reality and ideal. The concern is no longer limited to young people. Adults across generations are increasingly worried about its impact too.

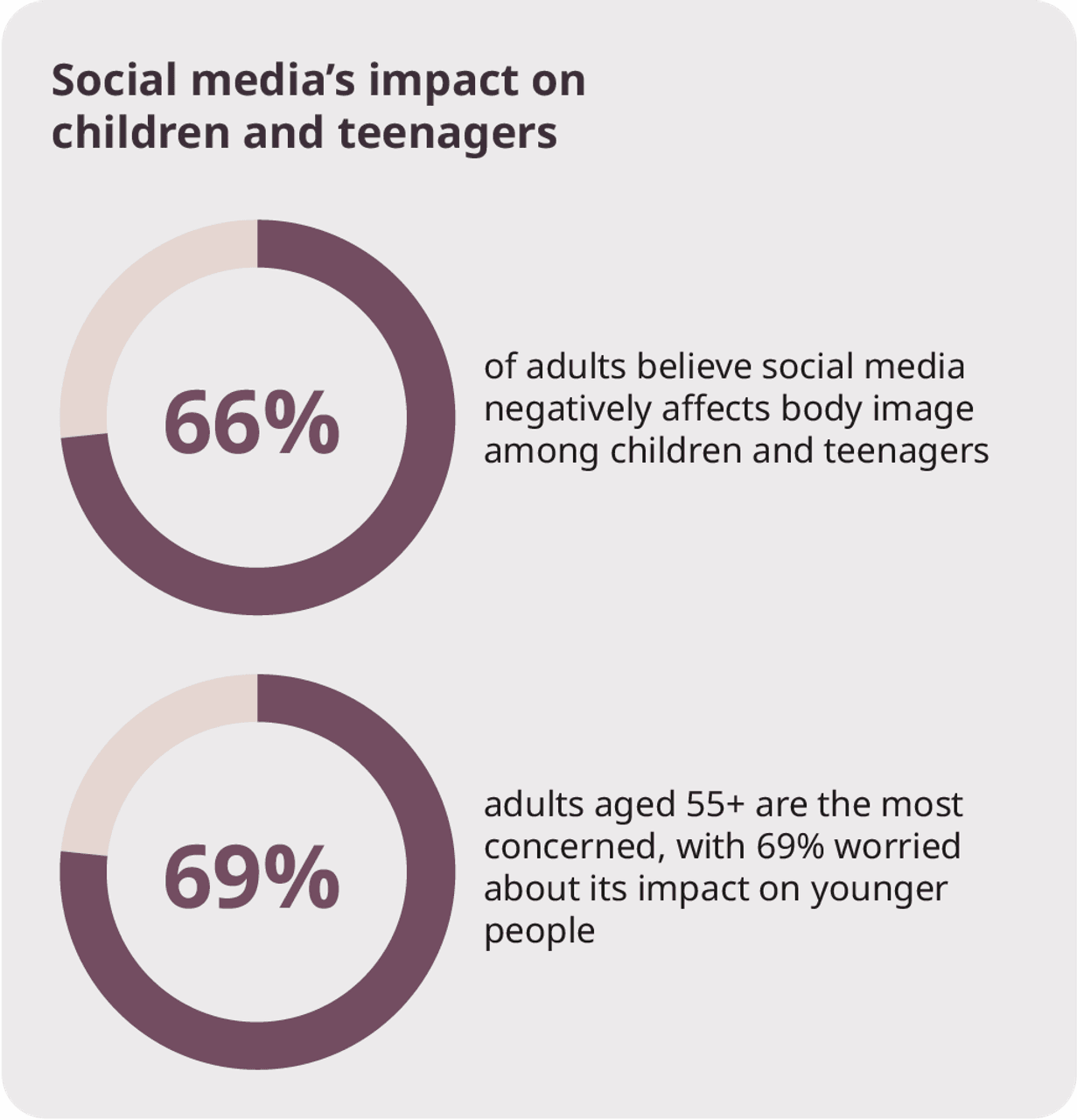
Social media is no longer viewed as a risk limited to teenagers. It is widely recognised as a cultural force shaping body image, confidence, and self-esteem across generations.
“Social media now plays a constant role in how bodies are seen and judged, often blurring the line between reality and ideal through filters and algorithm-driven content. What is increasingly clear is that this pressure affects adults as well as children, shaping confidence, body image, and attitudes to weight across generations. That is why clear, honest education and supportive, non-judgemental weight management matter more than ever.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Filters and AI
As technology advances, the line between real and edited bodies is becoming harder to see. AI tools and social media filters are no longer niche features. They are increasingly part of how people present themselves online, shaping expectations around appearance and intensifying pressure around weight and body image.
Changing behaviour:
- 19% of social media users now use AI to alter their image before posting.
- This rises sharply among younger users, to almost two in five of Gen Z and over one in three (34%) millennials.
Rising concern:
- More than 56% of adults believe AI and social media filters are making pressure around weight and body image worse.
- Concern is higher among women, with 59% saying filters and AI are increasing pressure.
Generational awareness:
- Millennials (58%) and Gen X (55%) are the most likely to flag filters and AI as a problem.
- These generations are both heavy social media users and parents, placing them at the intersection of use and concern.
Parents feel it most:
- 59% of parents with children at home are worried about the impact of filters and AI.
- Concern remains high even among non-parents, with 55% expressing worry.
Our data suggests that AI and filters are not just changing how images look, but how bodies are judged. As altered images become more common, pressure around weight and appearance risks becoming normalised, particularly for younger generations growing up in increasingly curated digital spaces.
“AI tools and filters are making it harder to tell where reality ends and editing begins. As altered images become more common, expectations around bodies and weight are shifting, particularly for younger people who are growing up in highly curated digital spaces. Many adults recognise that this is adding to pressure and comparison rather than confidence, which is why helping people understand what they are seeing, and offering supportive, non-judgemental guidance around weight and health, matters more than ever.”
Niya Mansuri, myBMI weight management and obesity expert
Part 7: Understanding weight behaviour
How people engage with their weight matters as much as the number itself. Tracking weight or activity can be a powerful tool, helping people notice patterns, build momentum, and stay connected to their goals. But for others, monitoring can feel loaded, uncomfortable, or discouraging, especially when progress is slow or pressure is high.
Looking at how people track, avoid, or disengage from monitoring helps reveal where confidence sits, how supported people feel, and whether change feels achievable or overwhelming.
Weight monitoring
How often people weigh themselves offers insight into confidence, habits, and how comfortable they feel engaging with their weight day to day. For some, regular weighing provides structure and awareness. For others, it is something they actively avoid.
· On average, 18% of adults weigh themselves once a week, while just one in ten do so every day.
· 18–24 year olds are the most likely to weigh themselves daily (16%).
· Adults aged 55+ are the most likely to never weigh themselves at all (20%).
These patterns suggest that weight monitoring is closely tied to age, confidence, and how people emotionally relate to their weight, rather than being a simple or universal habit.
“Stepping on the scales is not a neutral act for many people. For some it offers clarity and control, while for others it carries anxiety, pressure, or a sense of failure when change is slow. The wide differences we see across age groups suggest that weight monitoring is less about discipline and more about how safe and supported people feel engaging with their weight at all. Understanding that emotional context is crucial, because lasting change is far more likely when people feel informed and supported, rather than judged or overwhelmed.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
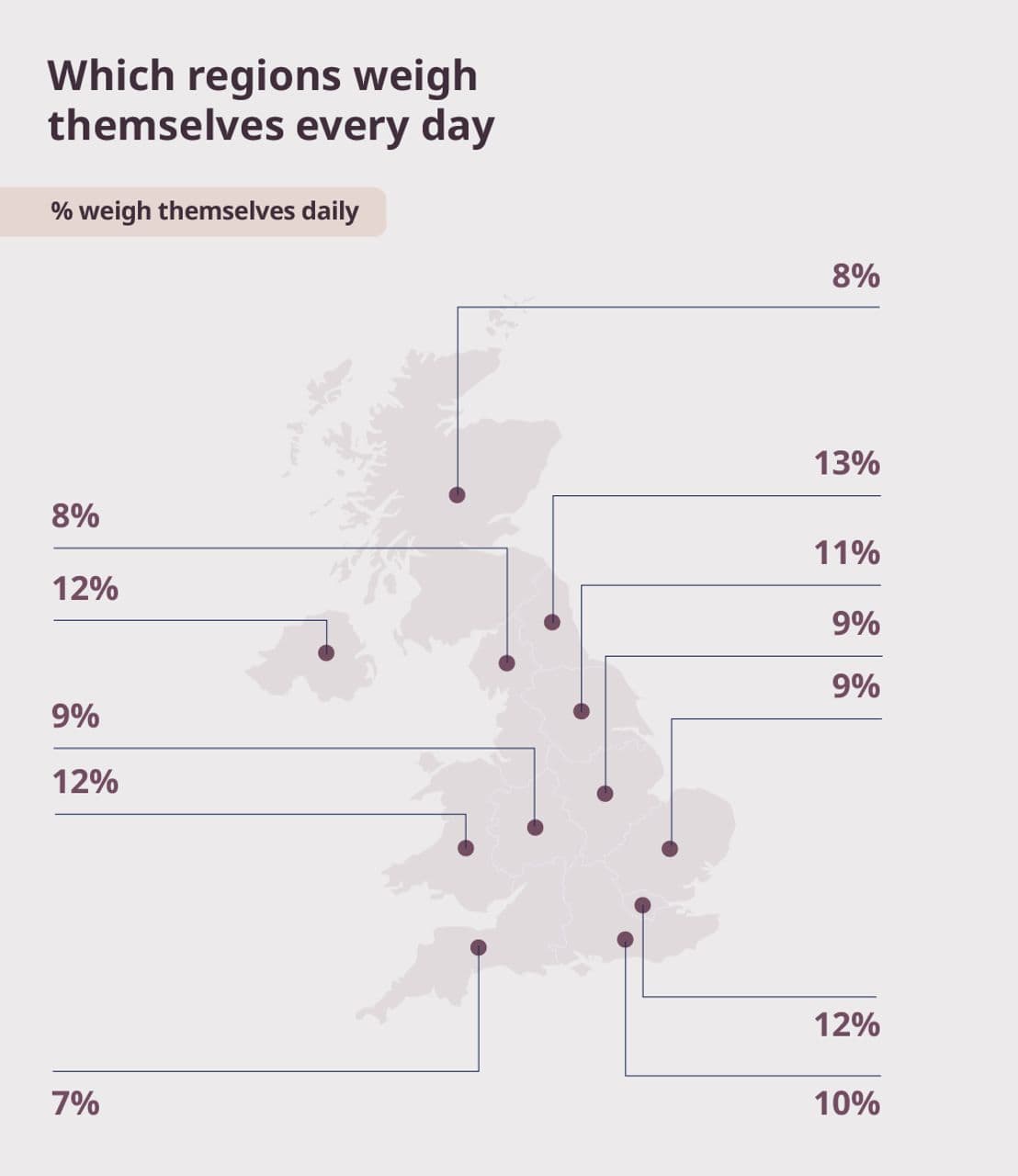
| Region | % weigh themselves daily |
|---|---|
| North East | 13% |
| Greater London | 12% |
| Wales | 12% |
| Northern Ireland | 12% |
| Yorkshire and the Humber | 11% |
| South East | 10% |
| East Midlands | 9% |
| East of England | 9% |
| West Midlands | 9% |
| North West | 8% |
| Scotland | 8% |
| South West | 7% |
Tracking our movement, activity and food
Tracking movement and food intake reveals how connected people feel to their health day to day. For some, it provides structure and motivation. For others, it is something they disengage from entirely, often reflecting confidence, routine, and how manageable change feels.
Daily activity tracking:
- 29% of UK adults track their steps every day.
- Women are more likely than men to track daily (32% vs 26%).
- Adults aged 45–54 are the most consistent trackers (34%), while 25–34 year olds are the least likely to track every day (28%).
- Those in a relationship are more likely to track daily (34%) than single adults (26%).
- On-site workers track slightly more consistently (31%) than those working from home (29%).
These patterns suggest that tracking is closely tied to routine and stability. Midlife adults and those in established relationships may be more likely to build tracking into daily habits, while younger adults appear less engaged with consistent monitoring, even when they are motivated to change.
Disengagement from tracking:
- More than one in three adults (36%) say they never track fitness goals.
- Adults aged 55+ are the most likely to never track activity.
- People working from home are less likely to disengage entirely, with just 19% saying they do not track any fitness goals.
This highlights a clear split. For a sizeable group, tracking feels irrelevant or unhelpful, while for others, especially those working from home, monitoring may offer structure in less predictable routines.
Food tracking:
- Just 17% of adults track their daily food intake.
- Those working from home are far more likely to track food intake (82%) compared with 64% of on-site workers who track their intake at some point.
Food tracking remains far less common than activity tracking, suggesting it feels more demanding or emotionally loaded. However, higher engagement among home workers points to the role of flexibility and control over meals in making monitoring feel possible.
“Tracking weight, steps, or food isn’t about willpower or effort alone. What we see clinically is that people are more likely to track when they feel supported, confident, and in control. For some, monitoring can be a really helpful tool that builds awareness and motivation. For others, especially when pressure is high, it can feel overwhelming or even discouraging. The key is helping people use tracking in a way that supports them, rather than adds another layer of stress.”
Niya Mansuri, myBMI weight management and obesity expert
People know what to prioritise, but struggle to sustain it
Despite the barriers they face, many people are actively trying to manage their nutrition. When asked what they prioritise for weight management, intentions are clear and largely aligned with public health advice.
Top nutrition priorities for weight management:
- 44% say they avoid takeaway or junk food
- 40% focus on reducing portion sizes
- 27% prioritise eating whole foods
- 25% track calories
How priorities shift across groups:
- Younger adults are more likely to track calories and engage with structured approaches.
- Older adults are more likely to focus on portion control and avoiding takeaway food.
- Lower-income groups are more likely to select fewer priorities overall, reflecting constrained choice rather than lack of awareness.
This shows that people largely understand what supports weight management. The challenge is not knowing what to do, but being able to maintain those behaviours in the context of cost, time pressure, and everyday life.
Part 8: Weight loss motivations
Weight change rarely happens without a reason. Behind every decision to lose weight or maintain it sits a mix of health concerns, confidence, life stage, and personal experience. Understanding what motivates people in 2026 shows where urgency is felt, where momentum already exists, and how priorities shift across age, gender, and region. These motivations help explain not just who wants to change, but why, and what kind of support people are most likely to respond to.
Motivation centres on change rather than maintenance:
- 54% want to lose weight in 2026.
- 32% want to maintain their current weight.
Motivation differs by gender:
- Women are more likely to want to lose weight (58%) compared with 49% of men.
- Men are more likely to want to maintain their current weight (35% vs 29% of women).
Midlife motivation is strongest:
Adults aged 45–54 show the highest desire to lose weight (60%).
This remains high among those aged 55+ (56%).
Motivation is lower, but still significant, among:
- 35–44 year olds (51%)
- 18–24 year olds (49%)
- 25–34 year olds (48%)
Medical support is linked to higher motivation:
- 65% of people using weight loss injections want to lose weight in 2026.
- This compares with 48% of non-users.
Motivation to manage weight in 2026 is widespread, but not uniform. It peaks in midlife, differs by gender, and is strongest among those already engaging with medical support.
“The desire to lose or manage weight is usually tied to a moment in life, a health concern, or a sense that something needs to change. That is why motivation is strongest in midlife, when priorities shift and long-term health feels more real. What this shows is that people are not lacking motivation, they are responding to where they are in life, and support works best when it meets them there.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
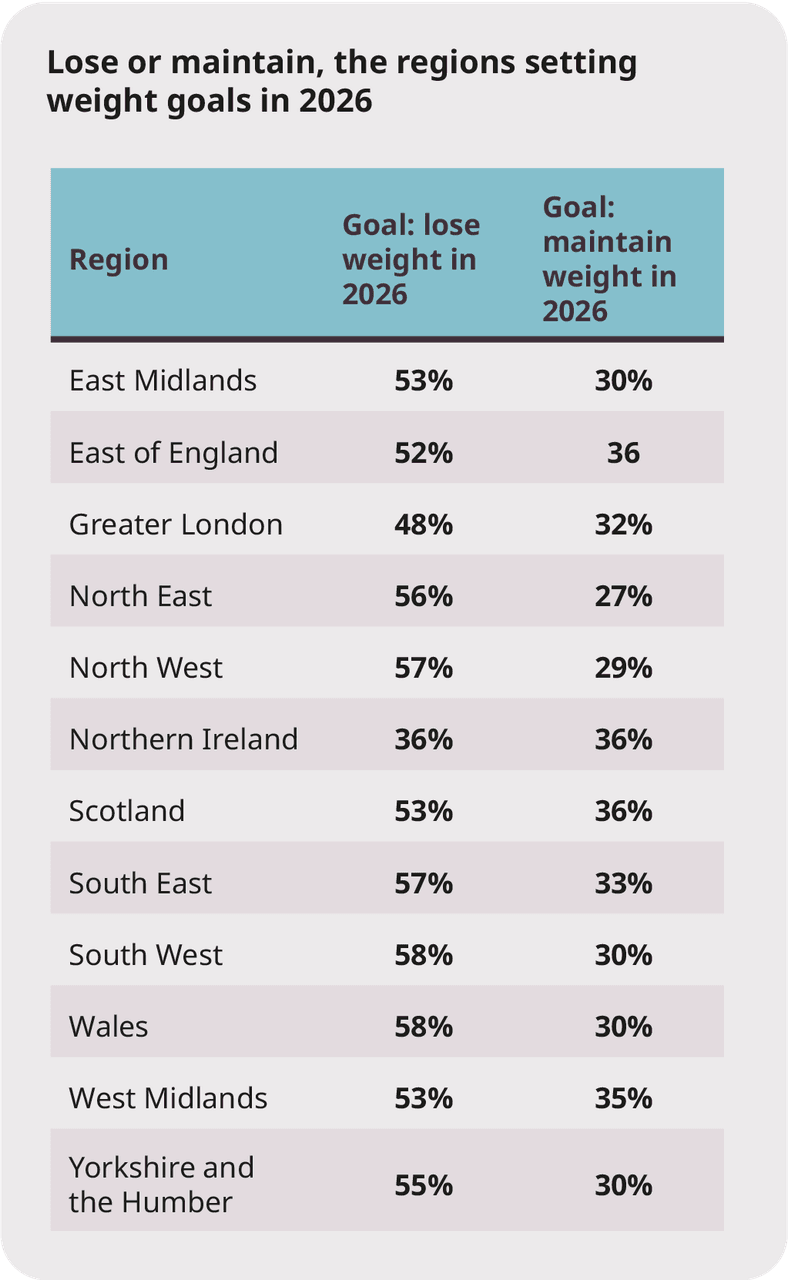
The reasons why we want to lose weight in 2026
Weight loss motivation in 2026 is largely about confidence, comfort, and quality of life, with clinical drivers playing a supporting, rather than leading, role.
How motivations differ by generation
While confidence and appearance matter across all ages, the primary driver for weight loss shifts by generation.
- Gen Z are most motivated by improving confidence (47%).
- Millennials (46%), Gen X (49%), and Baby Boomers (53%) are most motivated by wanting to look better in or fit into their clothes.
- The Silent Generation (80+) stands apart, with their biggest motivation being improving fitness (48%).
This highlights how younger adults are driven more by self-perception and confidence, while older generations place greater emphasis on comfort, appearance, and physical capability.
Top motivations to lose weight by region in 2026
Weight loss is often split across two main motivations, aesthetic and healthy lifestyle. Across most of the UK, the leading motivation to lose weight is appearance, but some regions place a stronger emphasis on fitness.
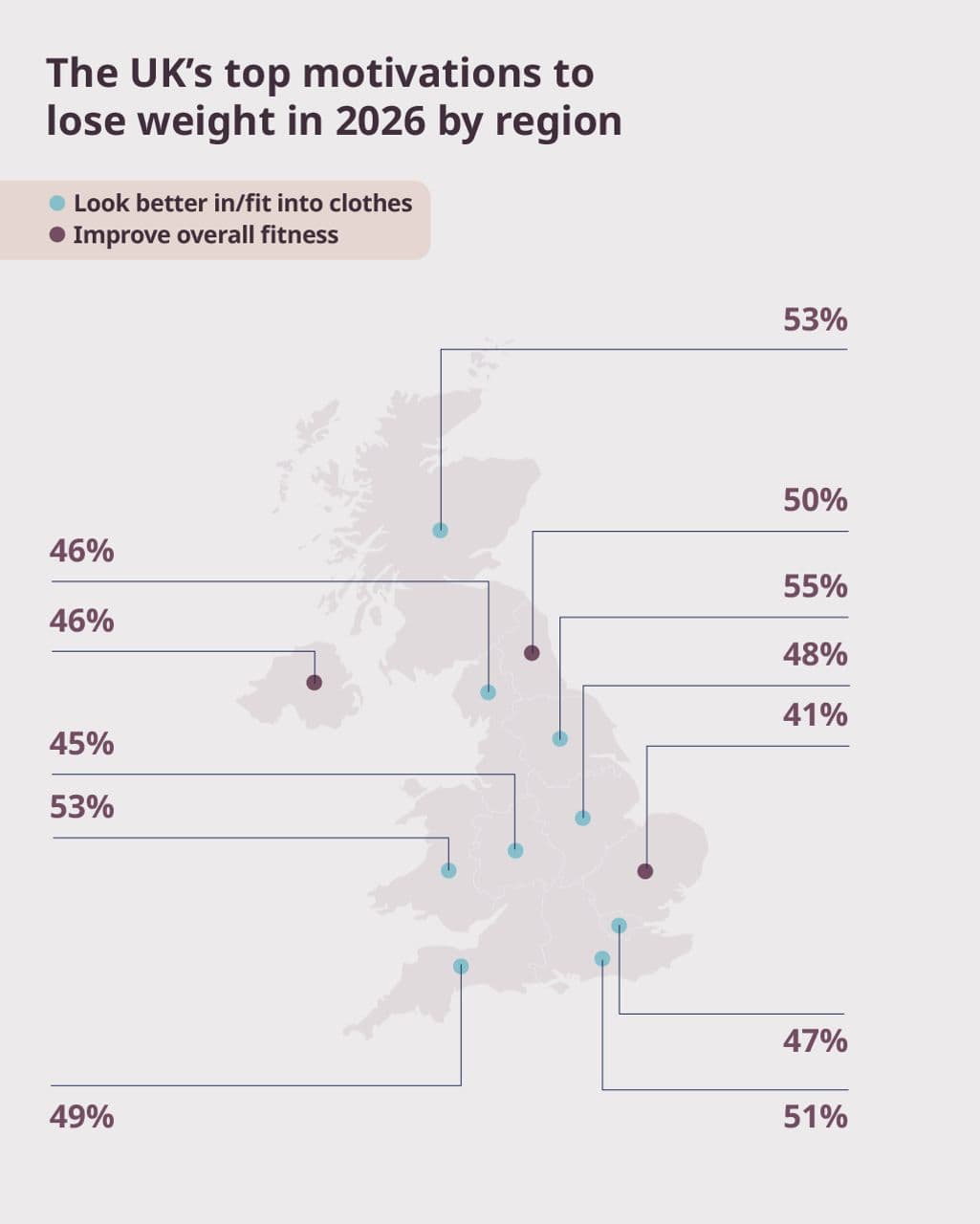
While confidence and fitness matter, the desire to feel comfortable in one’s own clothes remains the dominant motivation for weight loss across most regions of the UK in 2026.
Part 9: Changing attitudes to weight loss medication
Weight loss medication has moved decisively into the mainstream. What was once treated as a last resort or a controversial shortcut is now increasingly discussed as part of a broader, legitimate approach to weight management.
The data shows a clear shift in how people think about treatment.
Weight loss medication is increasingly seen as a support tool – not a shortcut
That acceptance comes with limits. Around 42% believe medication should only be used by people who have tried everything else, reinforcing the idea that it is still seen as a last resort.
Moral judgement has not disappeared either. One in 10 people (11%) say they are put off from using medication for weight loss for fear of being seen as “cheating”, and 12% are not sure they work, showing that stigma and lack of education continue to shape opinion.
What we’re seeing isn’t confusion – it’s change. People are still figuring out how weight loss medication fits into treatment. Most agree it works best alongside diet and exercise, not instead of it.
“What this shows is not confusion, but a shift in thinking. Many people still see weight loss medication as a last resort, and the idea of ‘cheating’ has not fully gone away, but attitudes are clearly evolving. Medication is increasingly understood as something that can support change, not replace effort, and work alongside diet and lifestyle rather than against them. When it is used safely and appropriately, choosing medical support can be a confident, informed step, not something people should feel the need to justify.”
Niya Mansuri, myBMI weight management and obesity expert
Public opinion is shifting
This matters because attitudes influence access, confidence, and willingness to seek help. As weight loss medication becomes more visible, the way it is framed will play a critical role in whether people feel able to consider it without shame or hesitation.
Medication - lived experiences
When people talk about their own lived experiences of weight loss medication, the tone changes. The focus shifts away from theory, debate, or headlines and towards how life actually feels day to day.
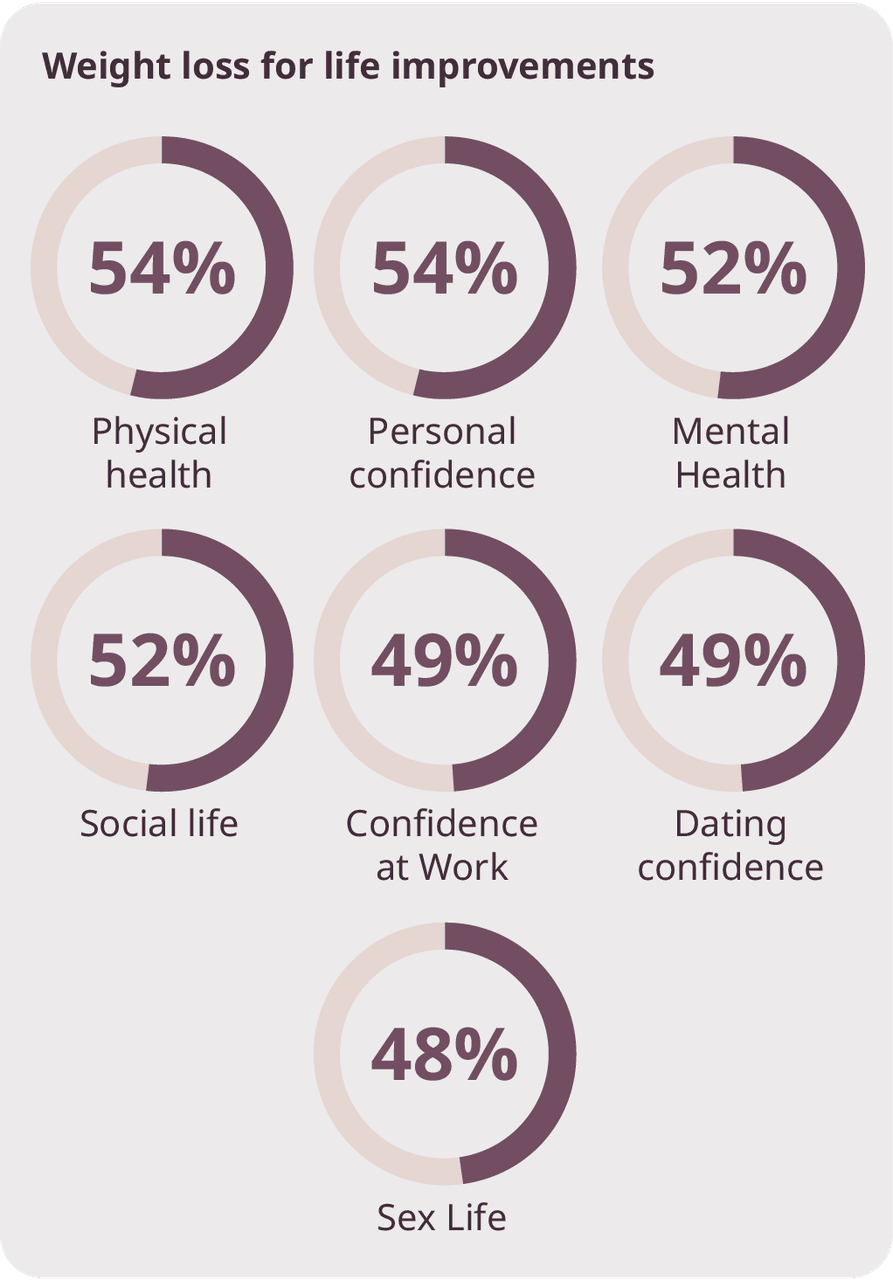
Across multiple areas, experiences are decisively positive. Just over half of users (54%) say their personal confidence has improved, while 52% report improvements in their mental wellbeing. People feel more in control, less consumed by constant decision-making around food, and better able to engage with everyday routines.
For many users, the biggest change isn’t physical - it’s mental load
The impact extends beyond private feelings. Nearly half (49%) say their confidence at work has improved, and 52% report a more positive social life. Confidence in dating also rises for 49%, suggesting that changes in weight management can influence how people show up in social and professional spaces, not just how they see themselves in isolation.
Even in more intimate areas, experiences tend to be positive. 48% say their sex life or intimate relationships have improved.
Physical health follows a similar pattern. 54% say their physical health has improved since using weight loss medication, compared with fewer than 12% who say it has worsened. This balance is consistent across all measures, pointing to benefit without widespread harm.
For most users, life feels better – not harder
Crucially, people do not describe medication as effortless or transformative on its own. Instead, it is framed as something that reduces friction. It makes healthier routines easier to sustain, rather than removing the need for effort altogether.
This distinction helps explain why attitudes are changing. For those who use weight loss medication, its value lies less in dramatic results and more in steadiness, consistency, and a sense that progress feels possible again.
The impact on mental and physical health is clear with 54% of weight loss injection users reporting improved personal confidence, 52% said they had experienced improvements in mental health and 54% have seen improvements in their physical health.
“People who use weight loss medication do not describe it as a quick fix or an easy option. What they often talk about instead is how it lowers the daily struggle, making healthier routines feel more manageable and progress feel possible again. That sense of steadiness matters. When effort starts to feel rewarding rather than exhausting, confidence grows, mental health improves, and physical health follows.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Part 10: Education is key to unlocking more choice
For many people, the decision to start a weight loss journey is shaped as much by understanding as by motivation. Knowing how medication works, what impact it can have on real lives, and how to access treatment safely all play a critical role in helping people feel confident about their options. When information is clear, trusted, and easy to navigate, people are better able to make choices that are right for them.
Education is not just about providing more information, but about delivering it in ways that feel credible, human, and genuinely useful.
“A lot of people are not short on willpower; they are short on clear information. When weight loss options feel confusing or hard to trust, it is easier to do nothing at all. Clear explanations, honest conversations with healthcare professionals, and guidance that is easy to understand give people the confidence to make choices that feel right for them.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
myBMI supports informed, confident choice
At myBMI, education is a core pillar, alongside nutrition, movement, and medication. It underpins how people understand their options, make decisions, and build genuine change over time.
Medication alone is not enough. People need clear, trusted information to understand how treatment works, what to expect, and how to use it safely as part of a broader approach to weight management.
Education at myBMI means:
- Clear, plain-English explanations of how weight loss treatments work.
- Expert-led consultations to support informed, medically appropriate decisions.
- Advice and guidance that reflects real life, not ideal scenarios.
- Ongoing support that sits alongside nutrition and movement, not separate from them.
This approach is built to help people feel confident in their choices, not rushed or pressured into them.
Aligned with the direction of NHS care
The importance of education also reflects the direction set out in the NHS’s 10-year plan, which places increasing emphasis on prevention, long-term condition management, and appropriate use of clinically proven treatments. As weight loss injections become more widely recognised as an effective option for some patients, there is a growing focus on safe prescribing, patient understanding, and long-term support.
Education as empowerment
For myBMI, education is about empowerment. When people understand their options, feel supported by healthcare professionals, and can access reliable information without judgement, they are better placed to make choices that work for them, now and in the long term.
Education is not a step in the journey. It is the foundation that connects nutrition, movement, and medication, and helps people turn access into lasting impact.
Part 11: Celebrating the positive impact of weight loss on our health
Weight loss is often reduced to numbers on a scale, but for people living through it, the real impact is felt day to day. It shows up in confidence, energy levels, relationships, and mental wellbeing, shaping how people move through their lives, not just how much they weigh.
For people who are currently using, have used, or are planning to use prescription weight loss injections, the picture is largely positive. Across every measure explored in this study, improvements are far more common than setbacks. These benefits are seen across ages, income levels, family situations, and regions, pointing to an impact that goes well beyond weight alone.
What this shows is simple.
Weight loss is not just changing bodies. It’s improving how people feel and function in their everyday lives.
Confidence improves across ages, incomes, and family situations
- 54% report improved confidence overall.
- This includes 23% who say their confidence has significantly improved.
Confidence gains are especially strong among younger and midlife adults, with those aged 18–34 the most likely to report significant improvements. However, positive changes in confidence are seen across all age groups, reinforcing that the benefits of weight loss extend well beyond appearance and into overall quality of life.
Social life improves alongside confidence
For many people, weight changes translate directly into how comfortable and confident they feel socially.
- 52% say their social life has improved overall.
- This includes 20% who report a significant improvement.
The impact varies by life stage:
- 18–34 yearolds are the most likely to report improved social lives, often linked to increased confidence going out or meeting new people.
- Nearly half of respondents report improvements in dating confidence (48%) and intimate relationships (48%).
These improvements are particularly pronounced among:
- Younger adults, where dating confidence improves most sharply.
- Single respondents, who are more likely to report increased comfort with visibility and attraction.
- People without children, who more often translate confidence into dating activity.
Among those in long-term relationships or later life stages, improvements are still common, but are more often described as feeling more relaxed, comfortable, and confident with a partner rather than increased social activity.
“What people describe isn’t a dramatic change in their social lives overnight. It’s more of a subtle shift. Feeling less self-conscious. Saying yes a bit more often. Being more comfortable being seen. For some, that means dating feels easier. For others, it’s simply feeling more relaxed with a partner or in social settings. Weight loss often gives people permission to take up space again.”
Niya Mansuri, myBMI weight management and obesity expert
Feeling better mentally, not just physically
Mental wellbeing also shows strong positive movement.
- 52% report improved mental health.
- This includes 21% who say their mental health has significantly improved.
How improvements are experienced differs by age:
- Younger adults are more likely to report improvements in mood and self-image.
- Midlife adults often describe reduced stress and greater emotional balance.
Across parental status, mental health improvement outweighs decline in every group, reinforcing that weight loss supports wellbeing across different family contexts.
“A lot of people talk about relief. Not constant happiness, but a sense that something heavy has lifted. Feeling more in control of their health seems to ease the mental strain they’ve been carrying, sometimes for years. Improvements in mood, confidence, and emotional balance show up differently at different stages of life, but the underlying feeling is the same: things feel more manageable.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Physical health improves, whatever your circumstances
Physical health shows the strongest and most consistent improvement of all outcomes measured.
- 54% report improved physical health overall.
- This includes 22% reporting significant improvement.
These gains are remarkably consistent across:
- Age groups
- Income levels
- Parental status
- Regions
People describe these improvements in practical, everyday terms:
- Parents often link physical gains to keeping up with children.
- Midlife adults report improved mobility and reduced discomfort.
- Older adults frequently say they feel steadier and more capable.
These physical improvements often act as the foundation for wider change, supporting confidence, activity, and longer-term progress.
“When people talk about physical changes, they rarely talk about numbers. They talk about everyday things feeling easier. Walking without thinking about it. Getting up without bracing themselves. Keeping up with their kids without feeling exhausted. Older patients often say they just feel steadier and more capable. Those changes matter because once the body feels less like a barrier, everything else starts to feel possible again.”
Niya Mansuri, myBMI weight management and obesity expert
How location shapes the positive impacts of weight loss
Weight loss delivers clear and consistent benefits across the UK. Improvements in confidence, social life, mental wellbeing, and physical health are seen in every region. Where people live does not determine whether they benefit, but it does influence how those benefits are felt and how quickly they build, often showing up as relief, reduced anxiety, and a greater sense of control over day-to-day life.
Regional data highlights:
- Over 53% report improved confidence across the UK.
- Over 51% report improvements in social life in every region.
- Over 52% report better mental health nationwide.
- Nearly 54% report improved physical health in all regions.
While experiences of weight loss may differ locally, the positive impact is widespread, consistent, and felt across the country.
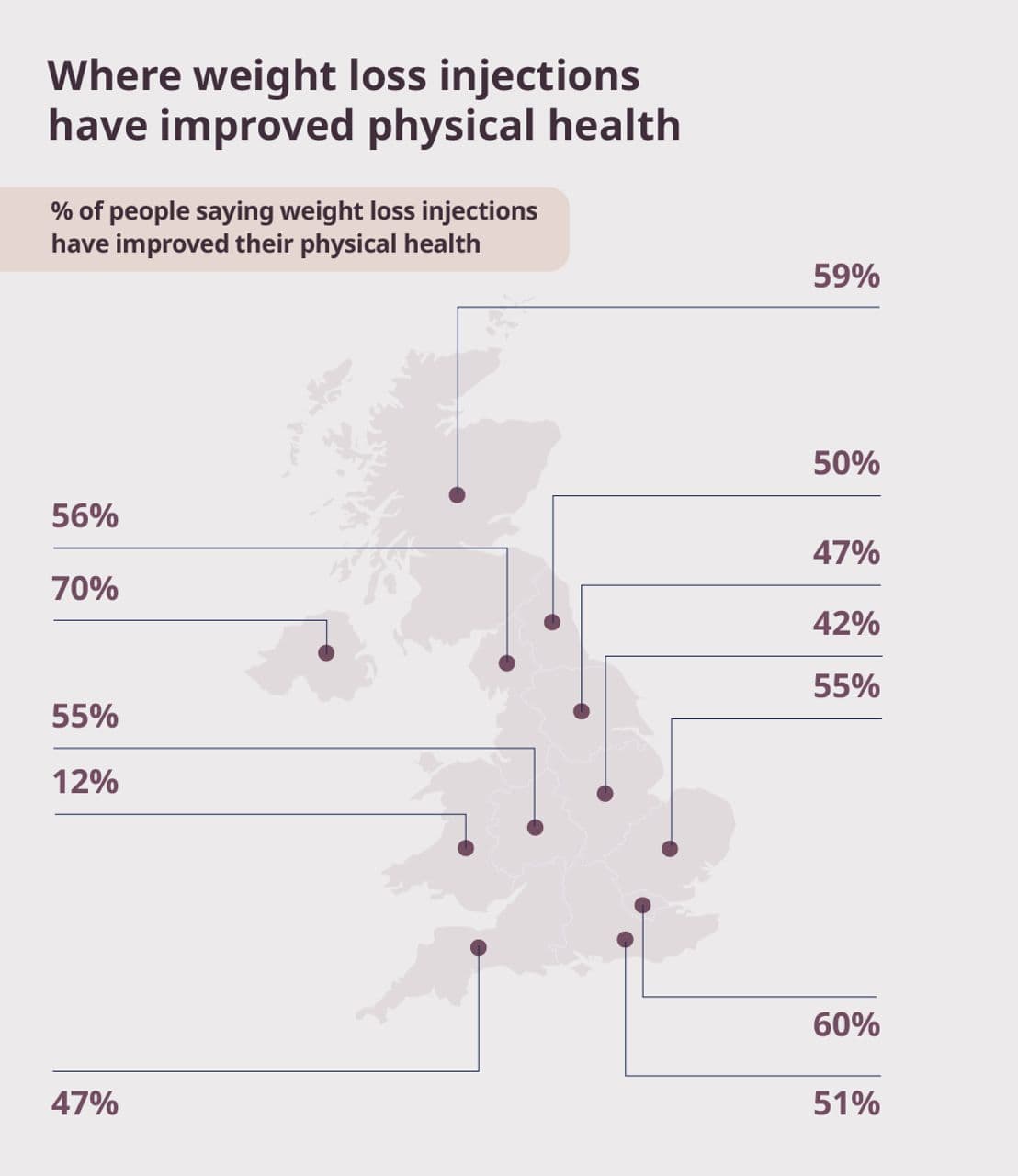
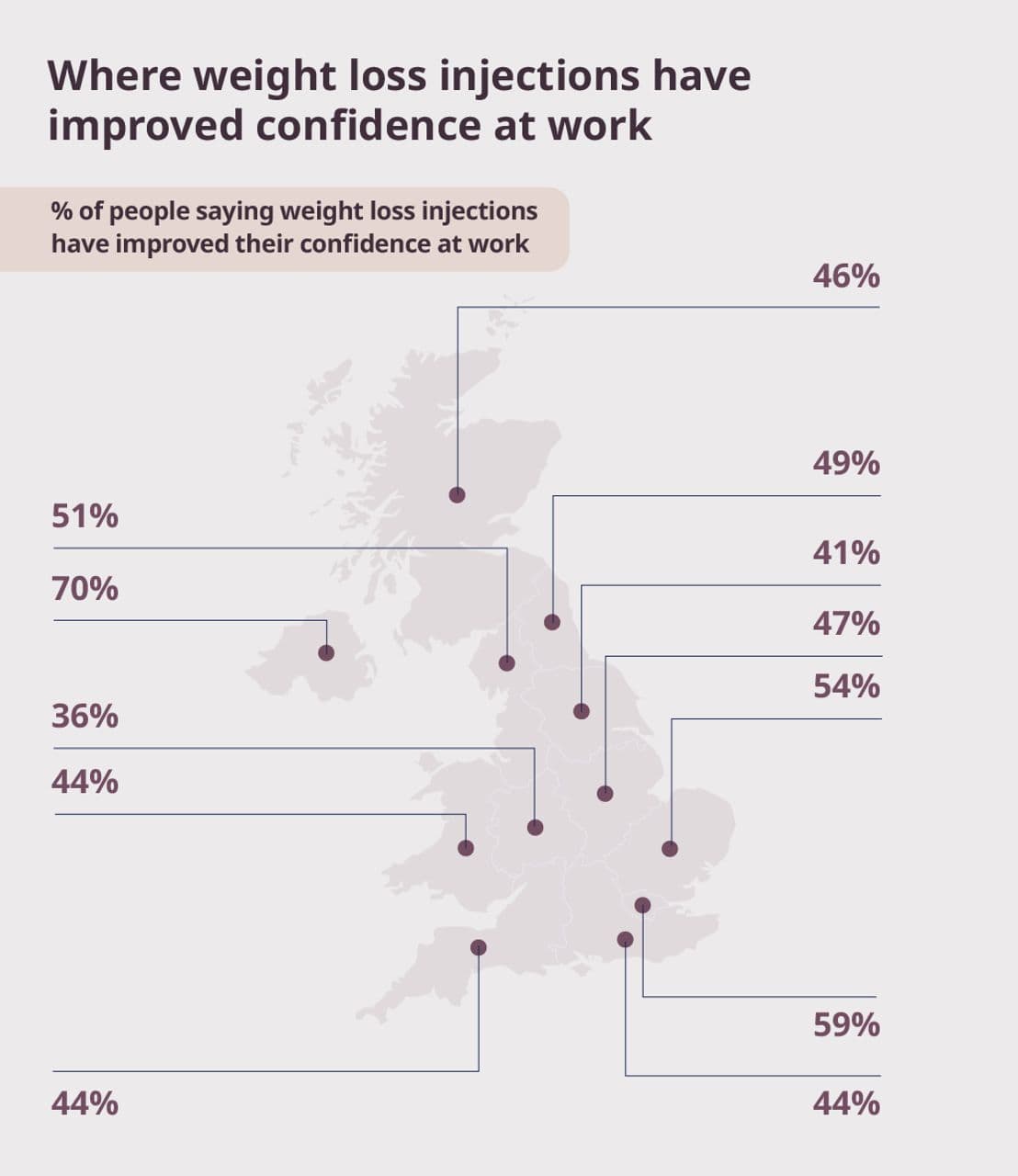
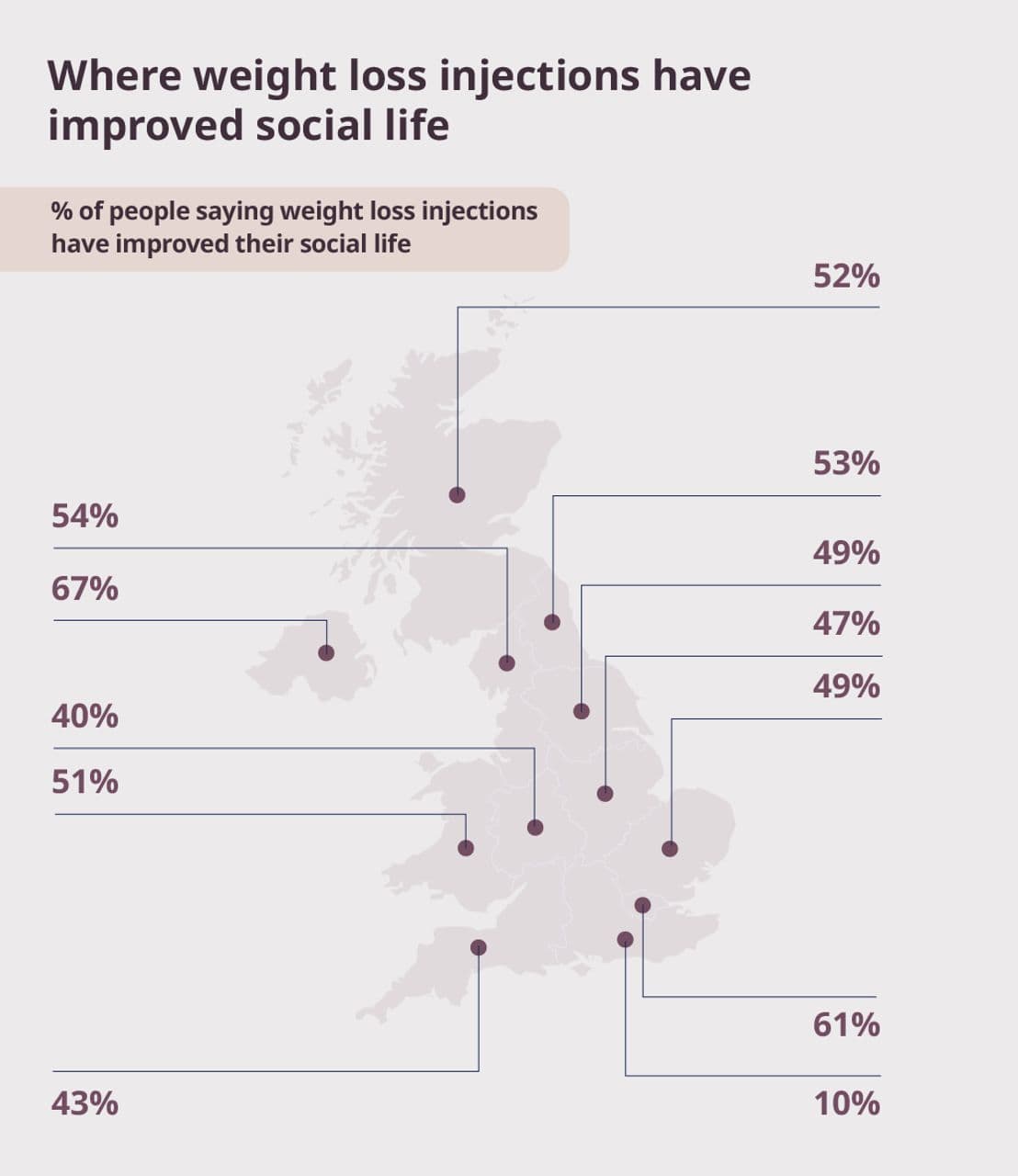
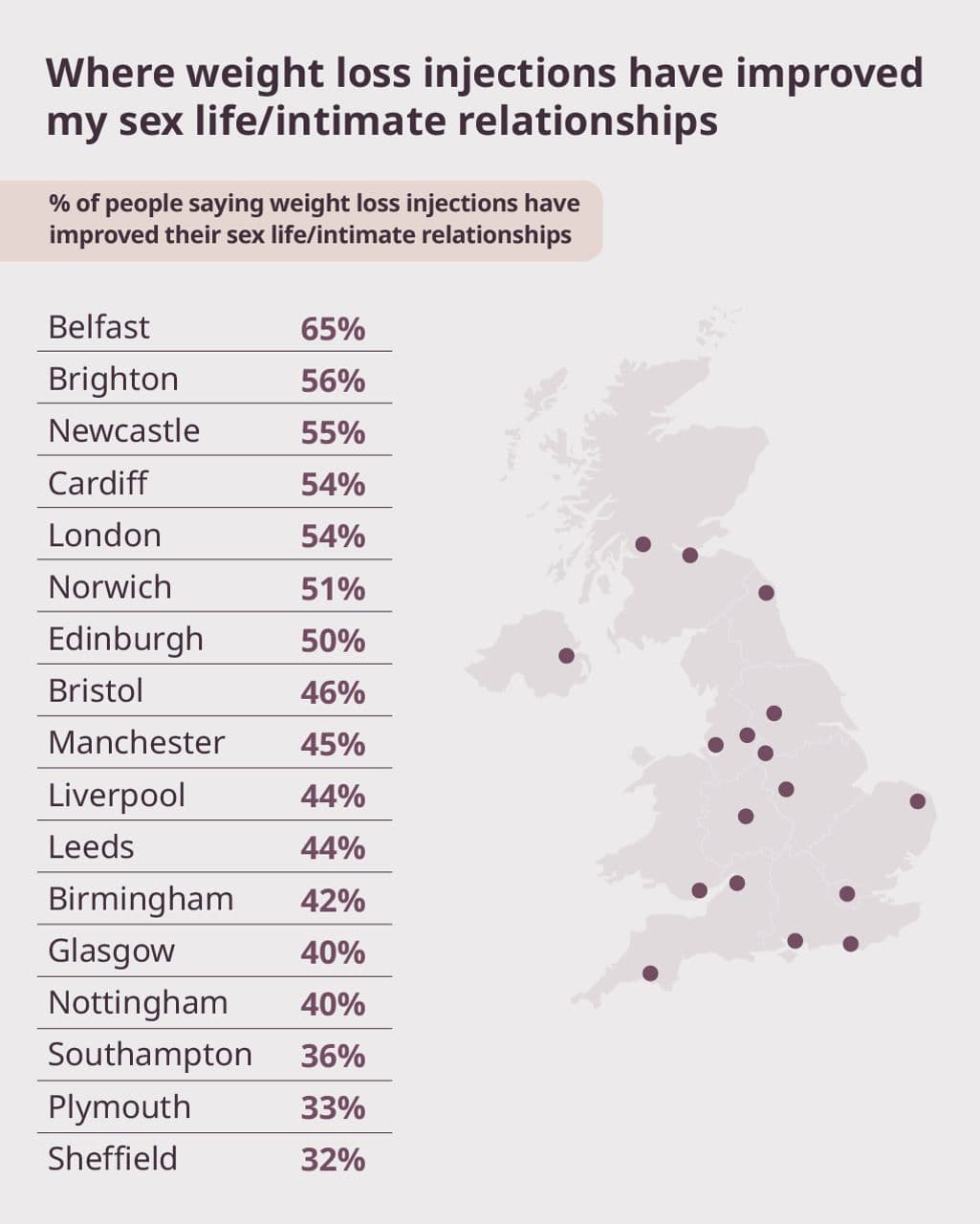
.jpg&w=3840&q=75)
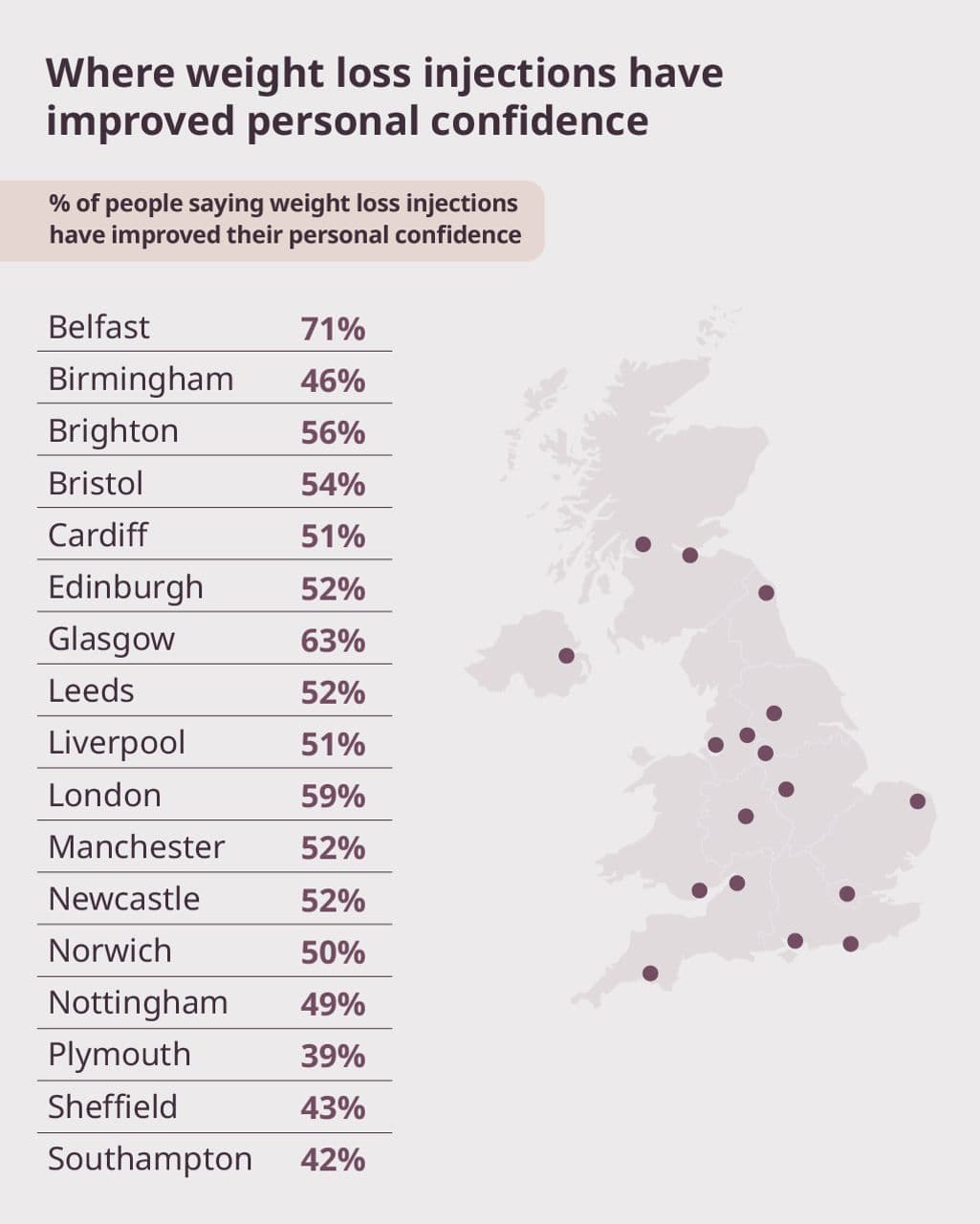
More than weight: positive change across real lives
Across every age group, income band, family situation, and region, improvement consistently outweighs decline. Weight loss is linked not just to physical change, but to greater confidence, stronger social connections, improved mental wellbeing, and better day-to-day health.
Where people live and how they live shape how these benefits are felt, but not whether they are felt at all. The positive impact of weight loss is widespread, meaningful, and deeply personal.
For myBMI, this reinforces a simple but powerful truth. Weight loss is not about chasing a number on a scale. It is about helping people feel more like themselves again. More confident. More capable. More present in their everyday lives.
Part 12: 2026: the year our relationship with weight changes
As the UK moves into 2026, the data shows a clear shift in how people think about their weight. This is not a year of hesitation. It is a year of intent.
More than 54% of adults say they want to lose weight in the next 12 months. A further 32% want to maintain their current weight. Weight loss is now the most common goal, marking a move away from standing still and towards taking action.
What makes this moment different is how widespread that intent is. The desire to change cuts across gender, region, income, and whether people are already engaging with medical support.
2026 could mark a turning point in the UK’s relationship with weight, driven not by pressure or stigma, but by clearer choices and growing access to support.
Weight loss becomes the majority goal
A clear majority of adults are planning to lose weight. When more than half the population shares the same goal, weight loss stops being a personal ambition and starts to reflect a broader moment of change.
Men and women are both engaged, but their goals differ
Both men and women are actively thinking about weight change heading into 2026, but the balance of their goals is different.
Men
- 49% want to lose weight
- 35% want to maintain their current weight
- 14% want to gain weight
This points to a broader mix of outcomes, including maintenance and strength-focused goals.
Women
- 58% want to lose weight
- 29% want to maintain their current weight
- 10% want to gain weight
Women are more likely to prioritise weight loss specifically, while men are more evenly split across loss, maintenance, and gain.
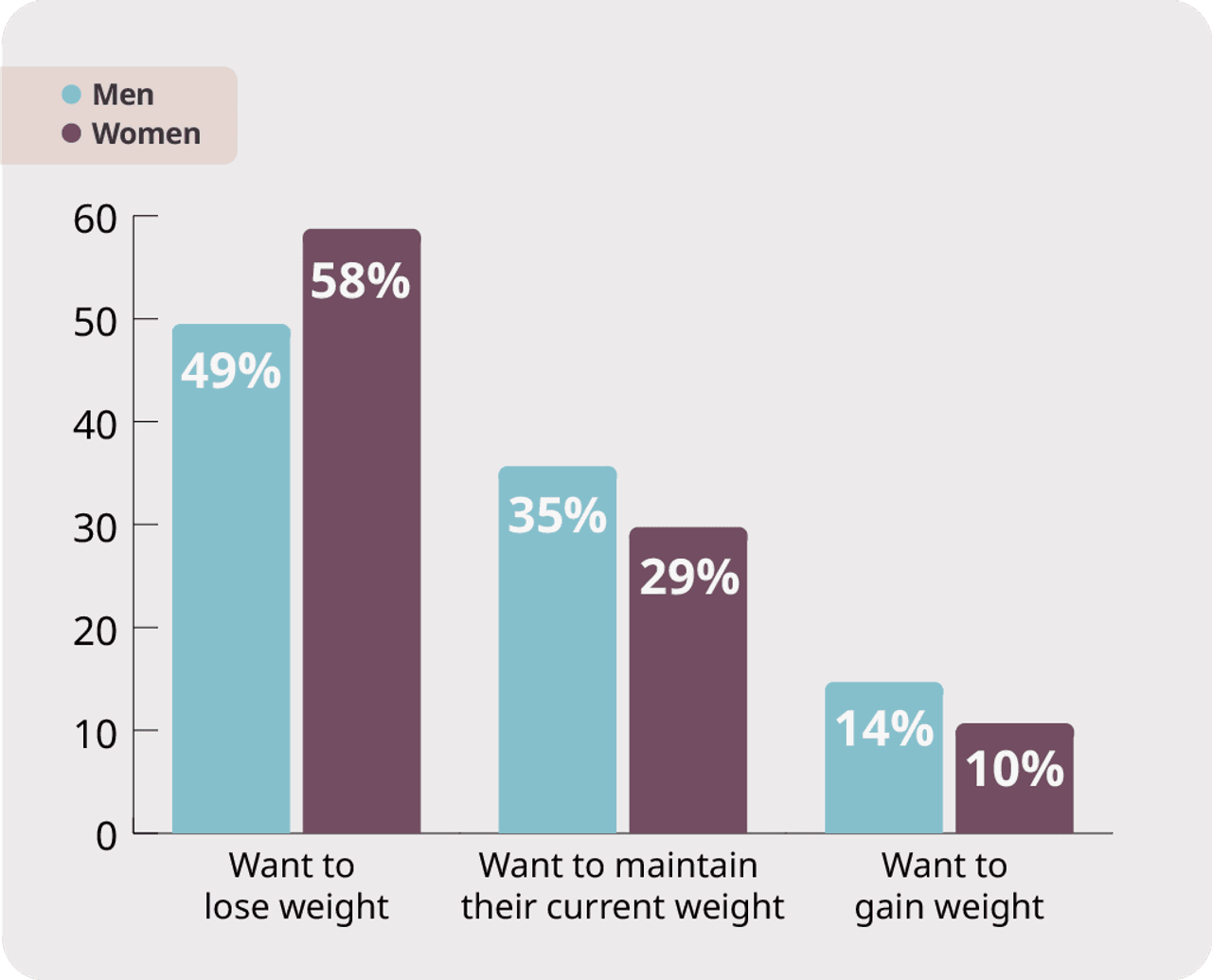
“Weight change is not a single goal. Some people want to lose weight, others want to maintain it, and some are focused on strength or overall fitness. What matters is that support reflects those different outcomes. When people have access to the right mix of medical guidance, nutrition advice, and movement support, they’re far more likely to work towards goals that actually fit their lives, rather than trying to force themselves into a one-size-fits-all approach.”
Ayesha Bashir, myBMI Obesity Expert and Prescribing Pharmacist
Geography shapes urgency, not motivation
Intent to lose weight varies across the UK, with the highest levels of motivation found in regions facing the greatest pressure.
The highest % of people looking to lose weight in 2026 are in Wales (58%) and the South West (58%) followed by the North West (57%) and the North East (56%).
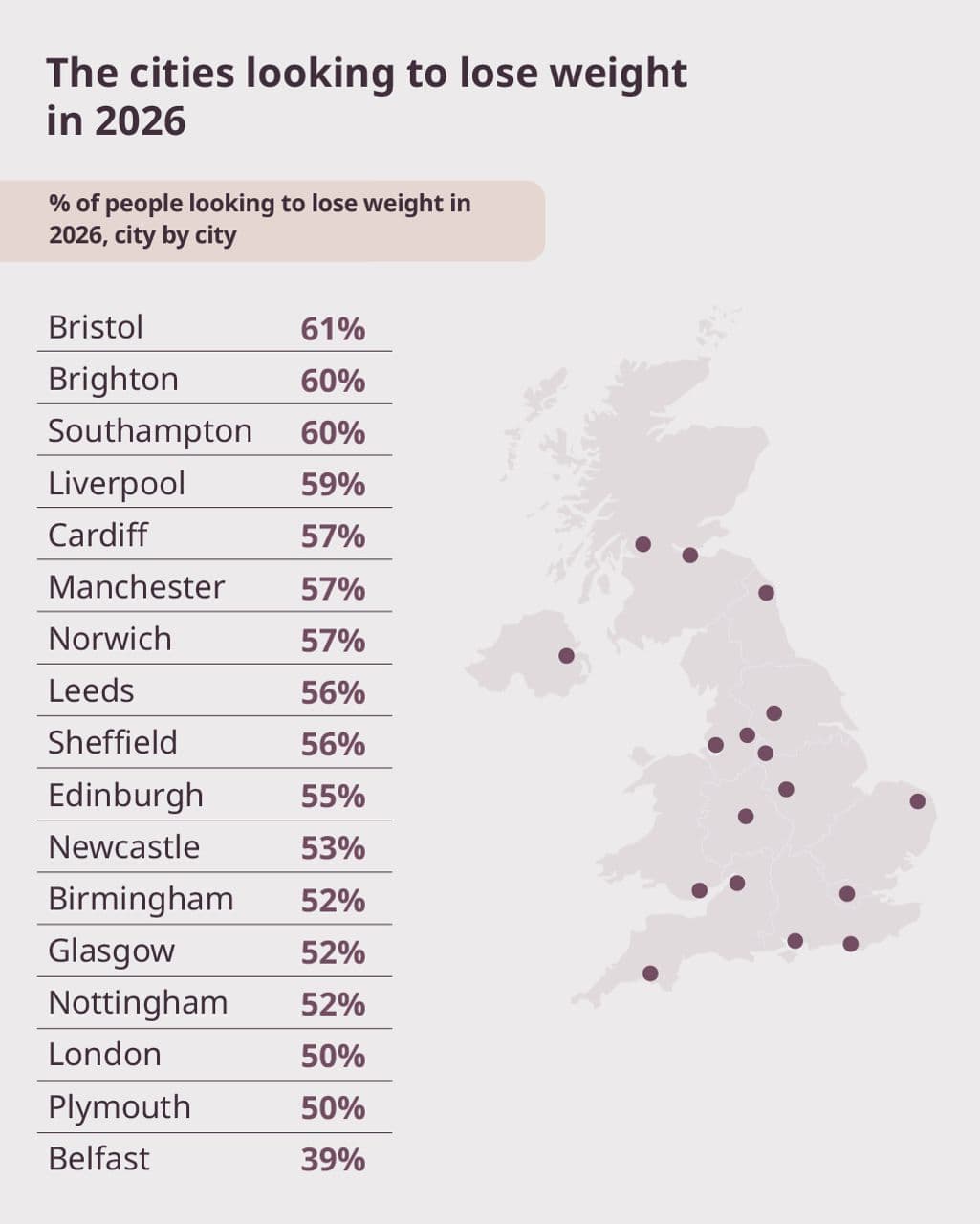
Weight loss injections and changing weight goals
The use of weight loss injections reveals important differences in how people approach weight change, shaping not just whether they want to lose weight, but how they think about maintenance, progress, and what comes next.
People currently using weight loss injections:
- 66% want to lose weight
- 16% want to maintain their current weight
This balance points to a shift away from short-term loss alone, towards longer-term weight management.
People who have used weight loss injections in the past:
- 81% want to lose weight
This is the highest intent to lose weight of any group, suggesting ongoing journeys or renewed determination.
People who have never used weight loss injections:
- 57% want to lose weight
This shows strong motivation even among those not currently using medical support.
What this shows
Weight change is rarely linear. People move between loss, maintenance, and renewed effort over time, and goals evolve as progress, confidence, and circumstances change.
A defining moment for 2026
Across gender, region, income, and stage of treatment, there's one clear picture. People are no longer disengaged or unsure. They are ready to act.
Weight loss is now the most common goal, but this shift goes beyond appearance or short-term targets. Men and women are equally engaged, working towards different but valid outcomes. Motivation is strongest where pressure has been felt the longest. And for many, medical support has reframed weight loss from a cycle of short-term attempts into a path towards stability, control, and long-term change.
This does not look like another year of starting over. 2026 marks a clear break from hesitation. People understand their options, and they are actively seeking support that fits their lives.
For myBMI, this is the moment that matters. Not just to help people lose weight, but to support change that works for real life.
A healthier relationship with weight. And progress that lasts.